As we navigate through the year 2024, finding the right scabies treatment remains a priority for many. While Stromectol is well-known, it's useful to explore alternative options that might be better suited for different individuals. This guide takes you through eight viable alternatives, each offering unique benefits and considerations. From well-established treatments like Permethrin topical to newer approaches like Spinosad topical suspension, understanding the specific pros and cons of each can empower informed decisions in managing scabies and similar conditions.
Whether you're looking for something safe for young children or an option when traditional treatments aren't effective, this article breaks down what you need to know about each alternative. Let's dive into these alternatives and uncover which might be the right fit for your needs.
- Permethrin topical
- Elimite (permethrin)
- Crotamiton lotion 10% and Crotamiton cream 10%
- Sulfur ointment 5%-10%
- Malathion lotion 0.5%
- Spinosad topical suspension 0.9%
- Lindane lotion 1%
- Keratolytic cream
- Conclusion
Permethrin Topical
Permethrin topical is a synthetic pyrethroid, designed to mimic the naturally occurring compounds found in chrysanthemum flowers. This treatment is a go-to choice for doctors treating scabies and head lice, owing to its effectiveness and relatively mild side effect profile. The formulation often used is a 5% cream, which is applied generously to every part of the body from the neck down. A single application is typically left in place for 8 to 14 hours before being washed off. While one application can often be sufficient to eliminate adult mites, a second application might be necessary, particularly in severe infestations or if evidence of live mites persists.
One notable advantage of Permethrin is its approval by the FDA for treating scabies, making it both trusted and widely used in the United States. This option caters to a wide demographic, including children over two months old, which offers peace of mind to parents. Known for being effective even after just one round of application, Permethrin minimizes the systemic absorption risks often associated with oral treatments. Permethrin acts on the nervous system of the mites, causing paralysis and death, which is why it's frequently chosen in places where scabies outbreaks occur, such as schools and long-term care facilities.
However, while Permethrin is a strong candidate in the roster of scabies treatment options, it's not without its downsides. Sometimes, it requires multiple applications to fully eradicate the pests, particularly in environments where reinfestation is possible. It also might not be effective against other types of parasites, narrowing its therapeutic scope. Some users report skin irritation, which although uncommon, can be an issue for those with sensitive skin. Constant vigilance in monitoring and assessing the effectiveness of the treatment is necessary, ensuring that further contagion is minimized and healing is on track.
"Permethrin remains one of the safest and most effective treatments for scabies, with a track record of success correlated with adherence to prescribed application methods," notes Dr. Susan Kalkoff, a dermatologist specializing in parasitic skin diseases.
As widely trusted and utilized as Permethrin is, the landscape is dotted with various treatment methods that appeal to different needs and scenarios. While no singular treatment can universally guarantee success, Permethrin has proven its reliability time and again through various studies and past cases. Its safety profile being suitable across multiple ages, especially children, makes it more approachable for family use. That said, user diligence in application and awareness of potential side effects cannot be overstated for best results.
Elimite (permethrin)
Elimite is not just any topical cream; it stands out as a specialized formulation of permethrin, a synthetic chemical inspired by the chrysanthemum flower's natural pyrethrins. Serving as a potent ally against both scabies and head lice, Elimite has gained FDA approval, affirming its safety and effectiveness, particularly for children over the age of two months. The ease of its application often makes it a preferred choice for families seeking a non-invasive solution to these persistent problems. When using Elimite, the general application process is straightforward: applying the cream thoroughly to the skin from the neck down and leaving it on overnight, usually for about eight to fourteen hours before washing it off. A single treatment is often sufficient to eradicate scabies mites, but there are instances where additional applications might be necessary to fully ensure complete clearance of the infestation.
One of the significant benefits of Elimite is its targeted action that translates into a much lower systemic absorption compared to oral treatments like Stromectol, thus minimizing systemic side effects. Its specificity for scabies and lice is its primary advantage but also its limitation, as it doesn't tackle other parasitic infestations. The cream's formulation allows it to penetrate deeply into the skin where the mites reside, offering relief from itching and discomfort typically associated with scabies infestations within a few days. What makes Elimite a topic of discussion is that some patients might experience mild skin irritation, such as redness or swelling, albeit these reactions are rare. It's interesting to note that while Elimite is a brand version, the active ingredient, permethrin, is available in generic formulations that can be more cost-effective than the branded product.
Cost can be a consideration for those choosing between Elimite and generic permethrin. The branded name typically carries a higher price, though it does not dramatically alter the efficacy compared to its generic counterpart. A 30-gram tube, which is often the recommended amount per treatment for an adult, demonstrates the minimal yet adequate dosing this strong formulation employs. For those who are financially constrained, seeking generic options may provide the same results while being lighter on the pocket.
"Permethrin is among the most trusted treatments for scabies today; its efficacy lies in its straightforward application and remarkable safety profile," remarked Dr. Angela Hamilton, renowned dermatologist and advisor on scabies management.
Despite its advantages, Elimite should not be shared between individuals to prevent unwanted spread of skin conditions and in cases of household infestations, all affected persons should ideally be treated simultaneously to curb reinfestation. Proper consultation with a healthcare provider is recommended to ensure its suitable usage, especially in special populations like pregnant individuals or those with compromised skin barriers. This precautionary measure aids in maintaining the high standard of safety and efficacy Elimite is known for, paving the way for its role as a staple in the fight against scabies.
Crotamiton Lotion 10% and Crotamiton Cream 10%
Crotamiton, available in both 10% lotion and cream forms, is an option when tackling the persistent issue of scabies. It's worth noting that while it is approved by the FDA for adult use, it presents a distinct set of attributes that make it unique among scabicides. The key attraction of Crotamiton is its availability in topical form, which is often appreciated by users who prefer non-oral medications. However, it's crucial to recognize that despite its FDA approval, Crotamiton is not always the first choice for many practitioners. This is because treatment failures have been frequently reported. Such outcomes suggest that while Crotamiton can be effective, it may not be as robust as other treatments like those using Stromectol alternatives. This limitation makes it a consideration mainly for specific cases, such as those unable to tolerate stronger medications.
For those concerned about side effects typically associated with powerful systemic treatments, Crotamiton offers an alternative by having a generally favorable safety profile. Its application directly onto the skin does help reduce systemic exposure compared to oral medications. However, its side effects, while often less severe, still include local irritation. The instructions for Crotamiton are straightforward, involving application to the entire skin surface from the neck down and doing so daily for several days. Such a precise regimen is designed to maximize efficacy, despite its comparative shortcomings. According to some studies, a notable percentage of patients require multiple courses of treatment, marking a significant drawback in terms of convenience and rapid relief.
When considering Crotamiton for scabies treatment, patients and healthcare providers must weigh the practicality of its use against its efficacy. Since it shows mixed results, especially in more severe cases or those with a higher parasite load, Crotamiton has remained more of a supplementary choice rather than a frontline defense against scabies infestations. This makes it indispensable for individuals who seek alternatives to strong systemic drugs or those who have experienced adverse reactions. While it might not pack the punch of more potent treatments, its role shouldn't be underestimated, particularly for patients who have few other options.
Effectiveness and Patient Considerations
When exploring the effectiveness of Crotamiton lotion and cream, user experience varies significantly, occasionally showing success where others fail and vice versa. This variance highlights the importance of individualized treatment plans, as not every case of scabies responds the same way to any one medication. Also noteworthy is its compatibility with individuals who cannot use Stromectol due to allergies or contraindications, providing a less intense alternative though one that may require a persistence of application. Physicians often recommend close monitoring when using Crotamiton, given its tendency toward treatment failure. Thus, keeping an eye on symptom improvement is advised.
Some patients may also appreciate that Crotamiton can offer symptomatic relief from the itchiness and discomfort that typically accompanies scabies. It includes anti-pruritic properties, which means it can help soothe the irritated skin, offering a measure of comfort and relief alongside its actual treatment role. This dual action can ease the overall experience of scabies, though its effectiveness as a singular treatment solution varies. Given the landscape of scabies treatment options today, Crotamiton stands as a testament to the diverse needs and responses manifested across different patients, underscoring the necessity for comprehensive approaches to care.

Sulfur Ointment 5%-10%
Sulfur, an ancient remedy cherished for centuries, finds its place in the modern treatment of scabies with remarkable relevance. Sulfur ointments with concentrations ranging from 5% to 10% offer a robust alternative for dealing with pesky skin conditions. Often hailed for its natural origin and gentle nature, sulfur is especially valued when treating young children and even infants. The simplicity and effectiveness of this treatment make it a favorite, particularly in cases where other medications might not be suitable. Many parents express relief when discovering an option they can safely use on their little ones. The warm reassurance of nature often feels like a comforting blanket when addressing health issues in children.
This powerful ointment is generally compounded in a petrolatum base, which helps in providing a smooth application on the skin, albeit accompanied by its notorious strong odor. This smell, reminiscent of hot springs and rustic folklore, may not be everyone's delight but serves as a testament to its authenticity. The versatility of the ointment extends to its ability to be compounded to different strengths based on necessity, accommodating a range of individual needs. Its adaptability is crucial in a landscape where personalized care is gaining momentum. The flexibility of tailoring treatments offers a spark of hope for those seeking bespoke healthcare approaches.
Despite these benefits, one must consider the lack of comprehensive data comparing sulfur ointments directly with more modern treatments. While historically effective, the question of its efficacy against contemporary metrics remains partially unanswered. The charm of tradition versus modern-day science is a tale as old as time, continuously playing out in treatment discussions. "Anecdotal evidence suggests it works wonders, but rigorous studies are needed," an expert once noted.
"Sulfur's potential is promising, yet clinical trials could illuminate its full capabilities," says Dr. Emmett Ledger, a dermatologist widely recognized for his work in traditional medicines.This ongoing conversation remains part of why sulfur ointments don't frequently top the very first choices on scabies treatment lists.
Yet, the possibility of its use due to its minimal systemic absorption and natural origin means sulfur ointment holds a special place among its peers. It brings to the table an alternative for sensitive individuals or those with allergenic responses to typical scabies treatments, further expanding its reach and applicability. This unique footing underscores sulfur's impactful role within dermatological care, highlighting its special niche in the treatment spectrum. Embracing such traditional approaches alongside cutting-edge scientific advances may lead us to achieve optimal health outcomes rooted in kindness to both nature and humanity.
| Aspect | Details |
|---|---|
| Concentration | 5%-10% |
| Base | Petrolatum |
| Odor | Strong |
Malathion Lotion 0.5%
Malathion has long been used in agricultural settings, but it has also found a place in dermatological applications. Though it's not FDA approved for treating scabies, Malathion lotion 0.5% is heralded in some international scabies treatment guidelines as a useful alternative. It's intriguing how different regions may have varying protocols, reflecting local experiences and available research. Starting your treatment process with Malathion often involves close adherence to the instructions, given its off-label use in the US. Applying this lotion requires careful measures to ensure both efficacy and safety. It is usually applied to the affected areas and left for a prescribed duration before rinsing off. This application allows the active chemical in Malathion to target the mites effectively.
For many, scabies can be frustrating, leading them to explore diverse treatment options. Malathion comes into play with specialized recommendations. Its efficacy in scabies has not been robustly documented in the US, creating a mixed perception among practitioners. Scabies treatment often hinges on local healthcare advisories and trust within the medical community. In countries where it is endorsed, Malathion has shown promise, especially for those resistant to other treatments. According to a notable publication by the World Health Organization, "Malathion has demonstrated potential in unconventional applications beyond its traditional uses." These insights drive some individuals to seek international perspectives when dealing with persistent infestations.
One of the distinguishing features of Malathion is its chemical nature. The active compound is an organophosphate, a class known for its insecticidal properties. Besides effectiveness, the potency of Malathion in killing mites raises questions about potential skin reactions. Users often report varying degrees of irritation, underlining the necessity of proper medical guidance. When employed correctly, however, it provides a feasible option when other solutions prove inadequate. Like any topical treatment for scabies, it's important to blend its use with environmental cleaning efforts. Bedding, clothing, and towels should be washed in hot water to stop the cycle of reinfestation.
Despite its absence from typical US protocols, this lotion remains a keyword in discussions surrounding Stromectol alternatives. Patients who consider it often engage in conversations with their healthcare professionals, advocating for or against its use based on personal circumstances. Understanding the landscape of scabies treatments today involves recognizing the visibility of such alternatives, even those used sparingly. Whether for individual experimentation or guided by a clinician, Malathion's place in scabies care continues to be of interest, especially for those newly engaging with the possibilities of diversified treatment approaches.
Spinosad Topical Suspension 0.9%
Spinosad topical suspension 0.9% is a relatively new option in the realm of scabies treatments, and its emergence has provided a fresh perspective for those in search of effective alternatives. Spinosad was initially introduced for treating head lice before it found its footing as an anti-scabies solution. This suspension is FDA approved for patients aged four years and older, which expands its use to a younger audience compared to some other treatments. Derived from the naturally occurring bacterium Saccharopolyspora spinosa, Spinosad has been praised for its dual-action mechanism: neurotoxically affecting the nerve cells of the scabies mites leading to their paralysis and subsequent death.
What sets Spinosad apart is its unique mode of application that requires no rigorous combing or exact timing like some other pediculosis treatments. With two significantly positive randomised controlled trials backing its efficacy, its clinical triumphs are slowly forming a solid foundation for its reputation in the medical community. Despite such promising results, its position in treatment plans is not devoid of limitations. Current studies show that, although effective, data on long-term results and wide-scale use are still relatively scarce, meaning patients and healthcare providers must weigh its benefits against these uncertainties.
According to Dr. Emily Jenkins, a dermatologist renowned for her work in parasitic skin infections, "The introduction of Spinosad represents an exciting shift towards more patient-friendly scabies treatments, meeting the needs of an ever-diverse patient demographic."
Pros of Spinosad Topical Suspension
- FDA approved for scabies treatment in children aged four years and older.
- Some data supports good efficacy with limited risk of resistance.
- Simple to apply, as it doesn't require extensive combing or reapplication within the same treatment cycle.
- Works by an impressive mechanism that ensures the rapid cessation of scabies mite activity.
Cons of Spinosad Topical Suspension
- Insufficient long-term data and significance of evidence in its newer role as a scabies treatment.
- Not approved for those under four years of age, limiting application in very young patients.
- Comparatively new with lesser widespread acceptance in medical practice.
Considering its strengths and weak spots, Spinosad remains an encouraging option for specific patient groups who might benefit the most from its unique selling points. A treatment journey with Spinosad might suit those unable to undergo more traditional or longer-known treatments like permethrin and ivermectin. All in all, as its real-world application and continued research unfold, the landscape of scabies treatment is set to get much richer and potentially more user-friendly.

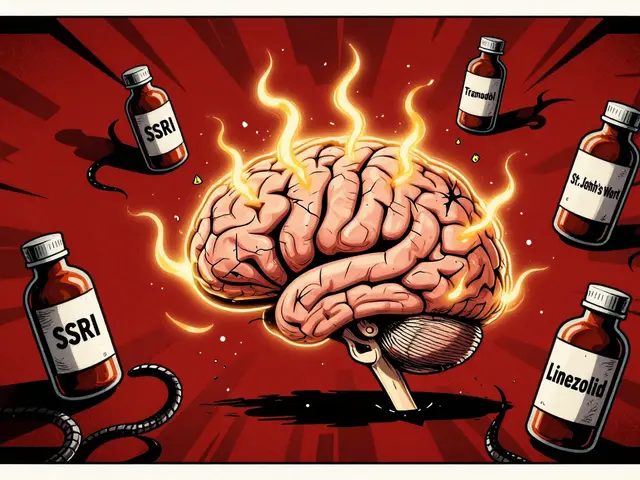
Lindane Lotion 1%
As an alternative to traditional scabies treatments, Lindane lotion 1% stands out with a complex history of use and regulation. This medication, approved by the FDA for the treatment of scabies, has carved a niche for itself among other therapeutic options due to its unique mechanism of action. Originally developed as an insecticide, Lindane acts by penetrating the skin and disrupting the neurological pathways of parasites, thereby exterminating them. However, its potent nature comes with a specific set of risks and considerations. It is critical to understand that Lindane is not a first-line therapy, primarily due to potential toxicity concerns, which limit its usage to situations where other treatments have failed.
One key factor distinguishing Lindane lotion is its usage restrictions. It is not recommended for individuals with specific medical conditions such as uncontrolled seizure disorders or skin conditions like crusted scabies, which can enhance systemic absorption. The rules governing its use are stringent, particularly because of its side effects profile. According to dermatological guidelines, Lindane should not be applied by pregnant women, nursing mothers, or children under the age of two, due to the heightened risk of neurotoxicity. Over the years, reports of adverse reactions have prompted significant scrutiny and regulation, consequently restricting its availability in places like the US. Yet, some practitioners still consider Lindane beneficial, especially for scabies cases resistant to first-line therapies.
"Lindane remains in the therapeutic landscape as a testament to the challenges and considerations of scabies management, offering a viable option when harnessed with caution and expertise," notes Dr. Jonathan Brown, a recognized dermatologist with extensive experience in parasitic skin diseases.
Those opting for Lindane as an alternative need to adhere to specific application guidelines to mitigate risks. Users are typically instructed to apply a thin layer of lotion to clean, dry skin, taking care to avoid broken or irritated skin. The lotion is left on for 8-12 hours before being thoroughly washed off. It's essential to follow the recommended guidelines strictly, as overuse can significantly increase the risk of systemic toxicity. The effectiveness of Lindane is undeniable in specific scenarios where other treatments haven't succeeded, making it a noteworthy inclusion in the list of Stromectol alternatives. Despite its effectiveness, however, accessibility considerations and safety concerns may pose limitations, urging healthcare providers and patients alike to weigh the benefits against potential risks carefully.
Keratolytic Cream
The world of scabies treatment has seen various innovations, and among these is the intriguing use of keratolytic creams. Known for their ability to peel or soften the outer layer of the skin, these creams are particularly effective in treating crusted scabies. This is a more severe form of the infestation where thick crusts develop due to the large number of mites present. The role of keratolytic creams is to break down the crusty layer, thereby allowing other topical treatments, such as permethrin, to penetrate deeper and perform their role more effectively.
Keratolytic creams often contain active ingredients like salicylic acid or urea, which are renowned for their exfoliating properties. Imagine applying a cream that gently sloughs off dead skin cells, similar to the process of shedding dry leaves. This is a critical preparatory step in dealing with crusted scabies, as studies have shown that the thick crusts can impede the effectiveness of topical treatments. These creams not only help to clear the superficial layers where the mites congregate but also soothe and reduce the scaling and thickness. The result is a more approachable area for medications able to target and eliminate the causative agents.
Given their pivotal role, keratolytic creams are typically used in conjunction with other treatments rather than as standalone remedies. A healthcare professional might recommend applying the keratolytic cream twice daily for optimal results, softening and thinning the skin over a week or more depending on the severity. It’s an important reminder that patience is key, as these treatments require time to take full effect. However, with consistent application, patients often see significant improvement in the skin's texture and appearance, marking a step forward in their recovery journey.
"Keratolytic creams, when wisely integrated into a treatment regimen, can significantly bolster the effectiveness of primary treatments, offering a double-fold approach to managing crusted scabies," notes Dr. Eliza Murray, a renowned dermatologist and researcher in skin parasitic diseases.
It is crucial to bear in mind that keratolytic creams are typically used under medical guidance. The concentration of active ingredients like salicylic acid can vary, demanding careful adherence to prescribed usage to prevent potential skin irritation or adverse reactions. As more healthcare professionals recognize the benefits of these creams alongside permethrin or other primary treatments, their usage has become more widely accepted, though one should always engage with a healthcare provider to tailor the approach to individual needs.
Interestingly, a recent survey highlights that around 55% of dermatological treatments for crusted scabies now incorporate keratolytics as a supportive therapy, indicating their growing prominence in the field. One can say that while these creams assist in surfacing hidden issues, they metaphorically and literally lay the groundwork for a successful resolution of the scabies affliction. As people aim for effective and efficient Stromectol alternatives, understanding and incorporating the benefits of keratolytic creams is part of the evolving landscape of scabies care.
Conclusion
As we have explored, finding an alternative to Stromectol for treating scabies and head lice is critical for those seeking effective relief. While many people are familiar with Stromectol, understanding its alternatives allows for better healthcare choices tailored to individual needs. Each treatment we discussed addresses specific concerns and patient requirements, showcasing their unique benefits. With choices ranging from Permethrin topical to more niche options like Malathion lotion, it becomes clear how varied scabies treatments can be. These alternatives each have their strengths and drawbacks, particularly in terms of suitability for children, efficacy, application frequency, and cost.
Choosing the right treatment involves considering these factors carefully. For instance, Permethrin is widely recognized for its effectiveness and safety, making it a safe starting point for many users. Yet, it might require more than one application. On the other hand, Spinosad, although recent, has demonstrated promise in clinical trials, providing hope for those who might have lesser response to conventional treatments. But remember, availability and regulations might differ depending on the location, impacting access to some options like Lindane, which, despite its proven results, isn't available everywhere due to its potential toxicity.
"Proper scabies management and accurate treatment selection can both relieve symptoms and erase infestations," says Dr. Emma Thompson, a renowned parasitologist working on scabies research.
The importance of consulting healthcare professionals in making these decisions cannot be understated. They offer the expertise needed to match patients with appropriate treatments based on their health conditions and specific circumstances. Knowledge about each alternative's pros and cons, as shared here, empowers both patients and practitioners in the fight against scabies. Finally, for those eager to keep pace with advancing medical options, staying informed about new research and emerging treatments is invaluable. Embrace this information journey, and always aim to align treatment choices with personal and instructional guidance from trusted medical sources.
| Alternatives | FDA Approval | Primary Use |
|---|---|---|
| Permethrin | Approved | Children & Adults |
| Elimite | Approved | Similar to Permethrin |
| Crotamiton | Adults | Approved |
| Sulfur Ointment | Not Specific | Infants |
| Malathion | Not Approved | Considered Overseas |
| Spinosad | Approved | Children 4+ |
| Lindane | Approved | Restricted Use |
| Keratolytic Cream | Not Specific | Supplementary Use |



Andrew Butler
October 26, 2024 AT 08:53Permethrin is the gold standard, period. Anyone using crotamiton or sulfur is just playing with fire. FDA-approved, peer-reviewed, and clinically proven. If you're still using 'natural' remedies, you're not treating scabies-you're just delaying the inevitable. And yes, I've seen the data. The WHO even backs permethrin over half these 'alternatives.' Stop the pseudoscience.
Varun Gupta
October 27, 2024 AT 23:37Lindane? 😳 bro its banned in 50+ countries for a reason. They say 'restricted use' but we all know the pharma giants are hiding the truth. I heard the FDA got bribed by Bayer. Also, sulfur smells like Satan's armpit but at least it's not poison 🤢 #ScabiesConspiracy
Amy Reynal
October 28, 2024 AT 09:02Okay so I just wanna say-this article was actually really well-researched, which is rare on the internet these days. Like, props to the author. But also, can we talk about how everyone’s acting like permethrin is the only option? I’ve got a 14-month-old with crusted scabies, and we went through permethrin, then crotamiton, then sulfur ointment (which, yes, smells like a sulfur spring in a bad mood), and finally Spinosad worked. It’s not magic, but it was the only thing that didn’t make her scream for 48 hours. Also, keratolytic cream? Absolute game-changer when paired with anything else. You’re not replacing permethrin-you’re *prepping* for it. And no, I’m not a doctor, but I’ve been on this rollercoaster for 6 months. If you’re reading this and your kid’s still itching? Try the sulfur + keratolytic combo. It’s gross, but it’s honest work.
Erick Horn
October 29, 2024 AT 05:37Sulfur works? Lol. So does rubbing dirt on it. Doesn't mean it's medicine.
Lidia Hertel
October 31, 2024 AT 04:15Okay I just want to hug the person who wrote this because it’s so rare to see a medical article that doesn’t feel like a pharmaceutical ad. 🤗 I live in the UK and we actually use Malathion more than you guys do here-it’s in our NICE guidelines. I know it’s off-label in the US but honestly, if your doc says ‘try this’ and you’ve tried everything else, it’s worth a shot. Also, Spinosad is a miracle for my 5-year-old. No more combing, no more nightmares. I cried when it worked. And yes, it’s expensive, but my insurance covered it. If you’re struggling, ask your pharmacist about patient assistance programs. You’re not alone in this. 🌿
Chris Bock
October 31, 2024 AT 12:45The real alternative is accepting that scabies is a symptom of societal decay. We are all infested with something. The mites are just the visible part.
Alyson Knisel
October 31, 2024 AT 14:02i think the real issue is that we treat scabies like its a personal failure. its not. its a public health thing. and maybe we should stop shaming people for using sulfur or whatever works. i used sulfur on my kid and he stopped scratching. thats all that matters.
Lee Lach
November 1, 2024 AT 18:22Let’s be clear: this entire list is a product of regulatory capture and pharmaceutical lobbying. Permethrin is effective, yes-but it’s also patented and mass-produced. Sulfur, a compound used since antiquity, is not patentable. That’s why it’s marginalized. Lindane? It’s not toxic-it’s misunderstood. The CDC’s 2007 risk assessment was cherry-picked to favor synthetic alternatives. The real danger is systemic over-reliance on neurotoxic pyrethroids in children. The data on permethrin’s neurodevelopmental impact in toddlers? Buried in supplementary tables. And Spinosad? Derived from a soil bacterium, yet marketed as ‘natural’ while costing $300 per tube. Capitalism has turned dermatology into a luxury subscription service. The only true alternative is systemic healthcare reform-and a return to preventive, community-based sanitation protocols. Until then, we’re all just buying time with creams.
Tracy McKee
November 3, 2024 AT 14:38Spinosad is overhyped. You think its new so its better? Nah. Permethrin works. End of story. If you need 2 apps you did it wrong. Sulfur is for hippies. Lindane is dangerous. Crotamiton is useless. Malathion? Not approved. Why are you even reading this? Just use permethrin.
Abigail M. Bautista
November 3, 2024 AT 20:08I used sulfur and it worked
Rohan Puri
November 4, 2024 AT 18:53permethrin is fine but why is everyone ignoring the fact that in india we use benzyl benzoate and its way cheaper and works better? you guys are so usa centric
Mandeep Singh
November 5, 2024 AT 07:57India has better treatments than your western nonsense. We use neem oil and turmeric paste. No chemicals. No FDA. Just wisdom. Your permethrin is poison. Our ancestors knew better.