When a doctor writes a prescription, they’re not just picking a drug-they’re making a decision that affects your health, your wallet, and their own income. Generic prescribing incentives are real, growing, and quietly reshaping how medications are prescribed across the U.S. These aren’t just formulary rules or insurance tricks. They’re structured financial and non-financial rewards that nudge providers toward cheaper, equally effective generic drugs. And if you’ve ever wondered why your doctor suddenly switched your brand-name pill to a generic, this is why.
How Incentives Actually Work
It’s not magic. It’s math. Generic drugs work the same as brand-name ones-they have the same active ingredients, same dosages, same safety profiles. But they cost 80-90% less. The U.S. spends over $250 billion a year on prescriptions, and generics make up 90% of all prescriptions but only 23% of total spending. That gap is where incentives come in.
Most health plans now use some kind of provider incentive. Blue Cross Blue Shield companies pay doctors $5 to $15 per generic prescription in targeted drug classes. Top performers can earn up to $5,000 a year just for choosing generics when appropriate. UnitedHealthcare’s Value-Based Prescribing Program saw generic use jump by nearly 25% in primary care. It’s not about forcing doctors to cut corners-it’s about rewarding smart, cost-conscious choices that don’t hurt outcomes.
But money isn’t the only tool. Some programs give priority scheduling to providers who consistently prescribe generics. Others speed up prior authorization requests. A few even offer recognition badges in their EHR systems. These small perks add up. Doctors are busy. Anything that reduces paperwork or speeds up care feels like a win.
The Tech Behind the Push
Electronic health records (EHRs) are the silent enforcers. Most systems now default to generic options when a brand is selected. A 2020 Duke University study found this simple tweak increased generic prescribing by over 22 percentage points. No extra work for the doctor. No patient asking. Just a smarter default setting.
These systems don’t just push generics blindly. Good ones include clinical decision support. If a patient has a known allergy, a history of poor response, or a complex condition like epilepsy where brand matters, the system doesn’t auto-switch. It flags the case. The goal isn’t to replace judgment-it’s to support it.
But integration isn’t easy. Over two-thirds of health systems report EHR interoperability issues. Training staff takes time. One practice needed 15-20 hours of provider training to fully adopt the system. And not everyone’s on board. About half of failed implementations cite provider resistance, often tied to fears of losing clinical autonomy.

What Works Best-and What Doesn’t
Not all incentive models are created equal. Formulary tiering-where insurers put generics in the lowest-cost tier-is common but weak. It pushes patients to choose cheaper drugs, but doesn’t directly affect doctors. Studies show it only boosts generic use by 8-12%.
Direct provider incentives? That’s where the real change happens. When doctors get paid or rewarded for prescribing generics, usage jumps 20-25%. The difference? The incentive hits the person making the decision.
But there’s a catch. Some programs backfire. A 2023 JAMA study found that doctors in the 340B program-meant to help safety-net providers-prescribed generics 6.8% less often than others. Why? Because 340B lets them buy brand-name drugs at deep discounts. So they’re financially better off prescribing the expensive version. The system rewarded the wrong behavior.
Same problem in places where doctors dispense drugs directly. In England, researchers found physicians with dispensing rights prescribed 3.1% more expensive drugs per patient. When the provider profits from the drug, the incentive flips.
Provider Voices: Real Stories
On Sermo, a physician network, Dr. Michael Chen from California said the UnitedHealthcare program added $2,800 to his annual income with almost no extra work. "It felt fair," he wrote. "I was already prescribing generics for most patients. Now I got paid for doing my job right."
But not everyone agrees. Dr. Sarah Williams in Texas told a Medscape survey: "Some programs feel coercive. What if my patient needs the brand because of a rare reaction? Do I risk their health to hit a quota?"
Reddit threads echo that worry. "MedDoc2020" wrote: "Generic incentives work great for hypertension or diabetes. But when you’re managing someone with five chronic conditions and three drug interactions? One-size-fits-all doesn’t cut it."
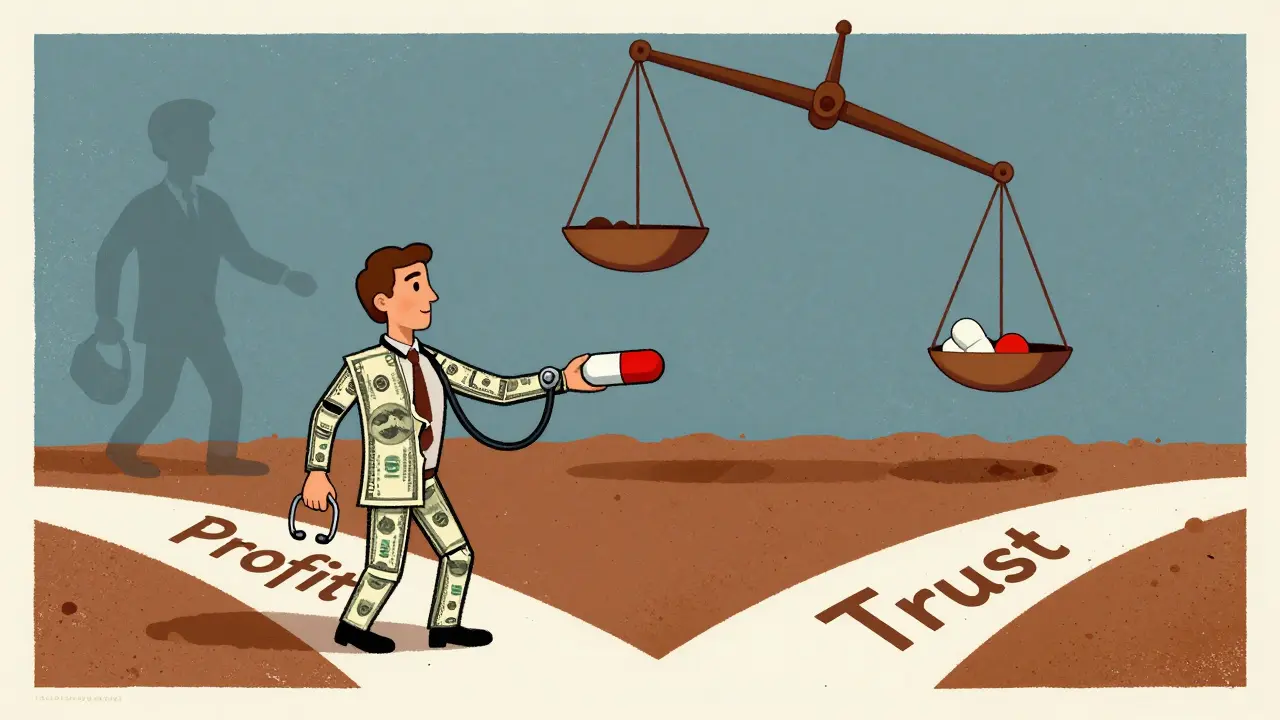
A 2021 MGMA survey found 63% of providers liked incentives when they were voluntary and tied to quality-not just cost. But 78% feared patient trust would erode if patients found out their doctor was being paid to prescribe generics. That’s the real tension: transparency vs. effectiveness.
Where the U.S. Stands vs. the World
The U.S. is catching up, but other countries are ahead. Germany uses reference pricing: if you prescribe a brand-name drug when a cheaper generic exists, the patient pays the difference. Result? 93% of off-patent drugs are filled as generics.
In the U.S., it’s 85%. And that gap is shrinking. CMS’s 2021 $2 Drug List-where essential generics cost just $2 at the pharmacy-boosted adherence by 17.3% among Medicare patients. The 2022 Inflation Reduction Act is pushing patent reform to clear the way for more generics. Experts predict generic use will hit 94% by 2028.
But it’s not just about price. It’s about structure. Countries with strong, centralized health systems can enforce uniform policies. The U.S. has 1,000+ insurers, hundreds of formularies, and fragmented data. That’s why the most successful programs here combine incentives with education, not just penalties.
The Bigger Picture: Savings, Risks, and the Future
Over the last decade, generics saved the U.S. healthcare system $1.7 trillion. The Congressional Budget Office estimates another $150-$200 billion in savings over the next ten years-if incentives are well-designed.
But poor design brings risk. A 2023 AMA survey found 61% of physicians felt burnout from tracking too many metrics. And if incentives push doctors to substitute drugs without clinical justification, patients can suffer. One study showed therapeutic substitution errors rose 12% in clinics with aggressive cost targets.
The future? Value-based contracts are coming. UnitedHealthcare’s 2024 rollout ties payments to both cost savings AND clinical outcomes. That’s the right direction. Not just "prescribe more generics," but "prescribe the right generic, at the right time, for the right patient."
Providers aren’t against saving money. They’re against being treated like vending machines. The best incentive programs don’t demand compliance-they build trust. They give doctors the tools, the data, and the autonomy to make the right call. And when they do, everyone wins: patients get affordable care, systems save billions, and doctors get rewarded for doing what they already know is right.
Do generic prescribing incentives lower the quality of care?
No, not when designed properly. Generics are required by the FDA to be bioequivalent to brand-name drugs. Studies show no difference in effectiveness or safety for most conditions. The real risk comes from rigid programs that ignore clinical nuance-like forcing a switch for epilepsy or thyroid medications where small formulation differences matter. The best systems use clinical decision support to avoid those cases.
How much money do doctors actually make from these incentives?
It varies. Most physicians earn $5-$15 per generic prescription in targeted classes. Top performers in programs like UnitedHealthcare’s can earn up to $5,000 annually. That’s not life-changing money, but it’s meaningful on top of a busy practice. For some, it offsets administrative costs or funds practice improvements. The key is that it’s tied to volume and appropriateness-not quotas.
Can patients find out if their doctor is being paid to prescribe generics?
Usually not. These programs are rarely disclosed to patients, and most providers don’t bring them up. That’s intentional-studies show disclosure can damage trust. But some ethical guidelines suggest transparency if the incentive is large or tied to specific drugs. The bigger issue is whether the choice is clinically sound, not whether the doctor got paid.
Are generic prescribing incentives legal?
Yes, they’re legal under current U.S. law. The Anti-Kickback Statute prohibits payments for referrals or to influence prescribing for specific drugs, but incentives tied to overall cost-efficiency and quality metrics are allowed. Programs must avoid rewarding the use of one specific brand over another. The focus must be on generic vs. brand, not which generic.
Why don’t all doctors use generics if they’re cheaper and just as good?
Some patients respond differently to formulations-even if the active ingredient is the same. Others have allergies to inactive ingredients. Some providers are used to prescribing a specific brand out of habit. And yes, some get paid by pharmaceutical companies to promote certain drugs. A 2016 Duke study found physicians receiving pharma compensation were 37% less likely to prescribe generics, especially in the first year after a drug goes generic.
What’s the biggest barrier to wider adoption of these incentives?
Provider resistance. Many doctors feel these programs treat them like robots. EHR integration is tough. Training takes time. And if the system doesn’t allow for exceptions in complex cases, it creates frustration. The most successful programs combine incentives with education, clinical flexibility, and transparent communication-not mandates.



Shanahan Crowell
January 2, 2026 AT 09:37This is wild-doctors getting paid $5 per generic? I didn’t realize it was that granular! And honestly? I’m all for it. If I’m getting the same medicine for 1/10th the price, why shouldn’t my doc get a little thank-you? It’s not bribery-it’s smart economics!
Plus, I’ve had my blood pressure med switched from brand to generic, and my BP hasn’t budged. My wallet? Happy. My doctor? Probably got a bonus. Win-win-win.
Why do people act like incentives = coercion? If you’re prescribing generics because they’re just as good and cheaper, you’re already doing the right thing. Now you’re just getting paid for it. That’s not a bug-it’s a feature.
And don’t even get me started on EHR defaults. I’ve seen systems auto-fill generics, and I’ve also seen them flag when a switch could be dangerous. That’s not robotic-it’s intelligent design.
Let’s stop pretending doctors are saints who never think about money. They’re humans. Give them a reason to do the right thing, and they’ll do it. Reward good behavior, not just punish bad.
I’ve seen practices where doctors get a badge in their EHR for hitting generic targets. It’s silly? Maybe. But it makes them feel seen. And that matters.
Also, the 340B loophole? Yeah, that’s a mess. But that’s a policy failure, not a failure of incentives. Fix the loophole, don’t kill the concept.
And hey-if you’re worried about trust? Talk to your doctor. Ask them why they chose a generic. Most will say, ‘Because it’s the same drug, cheaper, and I don’t want you to skip doses because it’s too expensive.’ That’s not shady. That’s caring.
Bottom line: incentives work. Bad incentives fail. But the idea? Brilliant. Let’s scale the good ones, fix the bad ones, and stop treating doctors like villains for wanting to be paid fairly.
Kerry Howarth
January 3, 2026 AT 11:04Generics are bioequivalent. The data is clear.
Shruti Badhwar
January 4, 2026 AT 12:19The structural inequities in U.S. pharmaceutical pricing are deeply entrenched, and while provider-based incentives represent a pragmatic intervention, they must be contextualized within broader systemic reform.
It is noteworthy that the financial remuneration for generic prescribing remains disproportionately modest relative to the scale of cost savings generated-often less than 1% of total savings accrued by payers.
Moreover, the absence of standardized metrics across insurers introduces heterogeneity in implementation, which may exacerbate disparities in care delivery, particularly in under-resourced settings.
The integration of clinical decision support within EHR systems, while commendable, is frequently hampered by interoperability constraints and vendor lock-in, which disproportionately affect smaller practices lacking IT infrastructure.
Furthermore, the ethical dimension of non-disclosure to patients warrants serious consideration: if the incentive is tied to clinical outcomes, transparency should be the default, not the exception.
Comparative analyses with Germany’s reference pricing model suggest that patient cost-sharing mechanisms may yield more sustainable adherence than provider incentives alone.
Nonetheless, the 25% increase in generic utilization under UnitedHealthcare’s program demonstrates that aligned incentives can drive measurable behavioral change.
The critical challenge lies not in whether incentives are effective, but whether they are equitable, transparent, and scalable without eroding clinician autonomy or patient trust.
Until we address the root causes of drug pricing inflation, we are merely treating symptoms with patchwork solutions.
Brittany Wallace
January 6, 2026 AT 03:50It’s so weird how we treat doctors like they’re supposed to be above money, but then act shocked when they respond to incentives 😅
Like, if you put a $5 bonus on doing something that’s already good for patients and cheaper, of course people are gonna do it more.
It’s not about controlling them-it’s about making the right choice the easy choice.
And honestly? I trust my doctor more when I know they’re not getting kickbacks from Big Pharma. Generic incentives? That’s like a ‘thank you’ from the system for not being a pawn.
Also, the EHR auto-switch thing? Genius. I didn’t even notice my med changed until I saw the receipt. No drama. No questions. Just… better care.
Let’s stop villainizing systems that save billions and make pills affordable. We need more of this, not less. 🙌
Michael Burgess
January 7, 2026 AT 09:35Man, I used to think doctors just picked drugs based on what they learned in med school. Then I found out some of them get free lunches from pharma reps and suddenly it all made sense.
But this? This is different. This isn’t shady. This is like a loyalty program for doing the right thing. $5 per generic? That’s like getting a coffee gift card every time you do your job right.
And the EHR defaults? I’ve seen them. You click ‘Lisinopril’ and it auto-switches to ‘Lisinopril HCTZ generic.’ No pop-up, no hassle. But if you’ve got a patient with a weird allergy or epilepsy? It flags it. It’s not forcing-it’s helping.
My cousin’s a PA in rural Ohio. She told me her clinic’s bonus from the Blue Cross program paid for a new ultrasound machine. That’s not ‘paying to prescribe.’ That’s ‘paying to care better.’
And yeah, some docs hate it. But that’s usually the same ones who get free pens and $500 dinners from drug reps. The ones who actually care about patients? They’re nodding along like, ‘Finally, someone gets it.’
Also, the 340B thing? That’s a loophole, not a feature. Fix that. Don’t throw out the baby with the bathwater.
Bottom line: if you want doctors to choose cheaper, equally effective meds? Make it worth their while. Not with bribes. With respect.
And if patients freak out when they see a generic? Tell ‘em it’s the same pill, just cheaper. Most of ‘em don’t care. They just want to feel better.
Also, the $2 drug list? That’s the real MVP. My grandma’s on it. She takes 6 meds. Now she’s not choosing between groceries and prescriptions. That’s not policy-that’s humanity.
Liam Tanner
January 8, 2026 AT 04:56Interesting read. I think the key is balance. Incentives are useful, but they need guardrails.
Hank Pannell
January 9, 2026 AT 15:05Let’s deconstruct the epistemology of pharmaceutical incentives: if we accept that clinical autonomy is a heuristic shaped by cognitive biases, then financial nudges are merely externalized heuristics designed to correct for market failures.
The 22% increase in generic prescribing via EHR defaults isn’t coercion-it’s algorithmic paternalism calibrated to minimize cognitive load while maximizing population-level utility.
But here’s the paradox: when providers perceive these systems as reducing their agency, even if objectively they’re enhancing decision quality, resistance emerges not from malice, but from existential threat to professional identity.
The 340B anomaly? Classic perverse incentive: when the agent’s profit motive aligns with the patient’s cost burden, the moral hazard becomes structural.
And let’s not conflate transparency with trust. Studies show disclosure doesn’t erode trust-it reveals the architecture of care. The real erosion comes from opacity, not incentives.
The German reference pricing model isn’t just superior-it’s a sociotechnical system where cost responsibility is distributed, not internalized solely by providers.
What we’re seeing isn’t a shift in prescribing behavior. It’s the emergence of a new clinical ontology-one where value, not just volume, defines therapeutic success.
Future iterations must integrate outcome-based metrics, not just cost. Otherwise, we risk replacing one reductionist model with another.
And yes, the $5 incentive? It’s symbolic. But symbols matter. They signal that the system sees you-not as a cost center, but as a steward.
Sarah Little
January 10, 2026 AT 13:41Actually, the data shows that when providers are incentivized to prescribe generics, they often overcorrect-especially in polypharmacy cases. The 12% rise in therapeutic substitution errors is alarming. This isn't just about money-it's about clinical risk. And EHR defaults don't account for pharmacokinetic nuances in elderly patients with renal impairment. You can't algorithmically optimize for bioequivalence when the patient's liver metabolizes drugs differently than the trial population. This system is dangerously oversimplified.
innocent massawe
January 11, 2026 AT 13:01Love this. In Nigeria, generics are the only option for most people. But we don’t have incentives-we have scarcity. If the U.S. can make generics the norm with smart systems, that’s huge. 🙏