Biologic DMARDs: What They Are, How They Work, and What You Need to Know
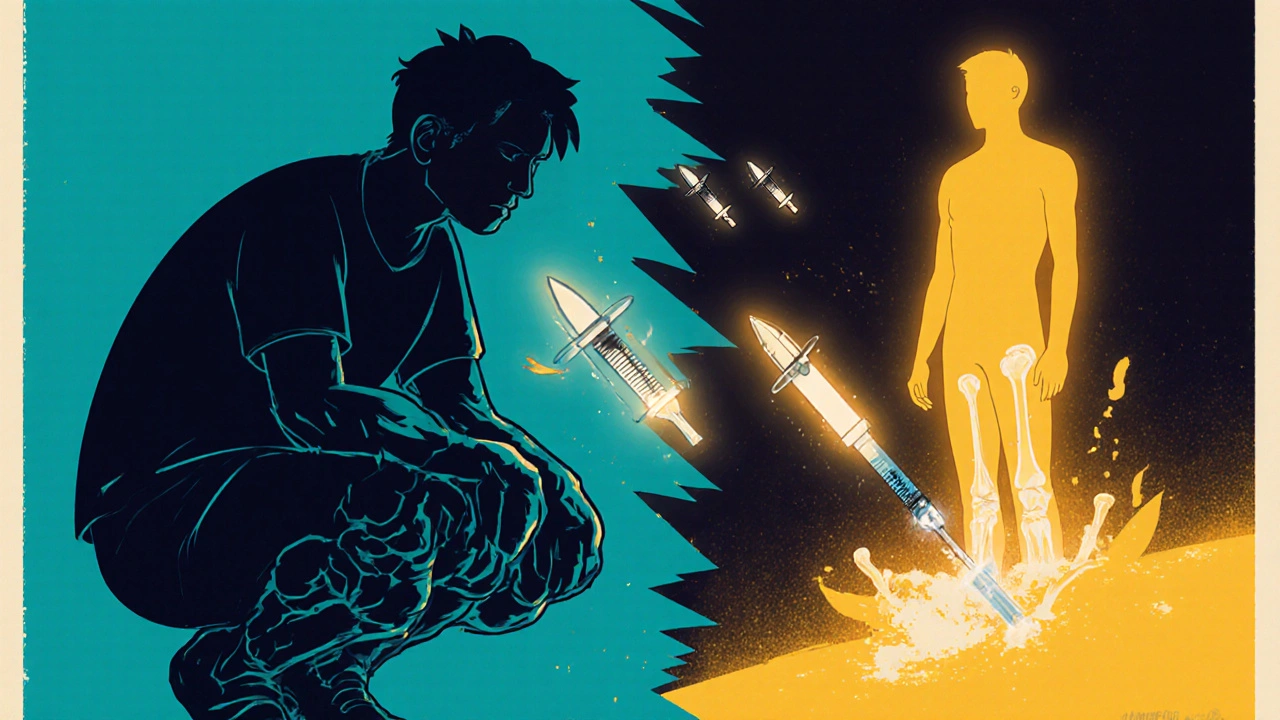
When your immune system attacks your own joints, skin, or organs, biologic DMARDs, a class of targeted medications designed to block specific immune system signals that drive inflammation. Also known as biologic response modifiers, they’re not your grandfather’s arthritis pills. These drugs are made from living cells and work like precision missiles—hitting only the troublemakers in your immune system, not the whole army. Unlike older DMARDs that suppress your entire immune system, biologic DMARDs zero in on molecules like TNF-alpha, IL-6, or B-cells. That’s why they work so well for conditions like rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease—but also why they come with unique risks.
These drugs are often used when traditional treatments like methotrexate fail. They’re not magic bullets, though. Many people see major improvement in pain and swelling within weeks, but others don’t respond at all. And because they dial down specific immune signals, your body becomes more vulnerable to infections like tuberculosis, hepatitis B, or even common colds. That’s why doctors always check for hidden infections before starting treatment. If you’ve had cancer, heart failure, or multiple sclerosis, some biologic DMARDs might not be safe for you. Monitoring isn’t optional—it’s built into the treatment plan. Lab tests, symptom tracking, and sometimes imaging are part of the routine.
There are different types of biologic DMARDs, and they’re not interchangeable. TNF inhibitors, like adalimumab and etanercept, block a key inflammation trigger called tumor necrosis factor. Anti-IL-6 drugs, such as tocilizumab, target a different pathway. Then there are B-cell depleters, like rituximab, which remove the immune cells that make harmful antibodies. Each has its own profile of benefits and side effects. Choosing one isn’t about which is "strongest"—it’s about matching the drug to your body’s specific immune behavior. Cost is another factor. These drugs can cost thousands a month, and insurance often requires trying cheaper options first. Some patients get help through patient assistance programs, but navigating that can be its own challenge.
What you won’t find in most doctor’s offices is clear advice on how to live with these drugs long-term. You need to know how to spot early signs of infection, when to skip a dose if you’re sick, and how to talk to your pharmacist about interactions with supplements or over-the-counter meds. You’ll also need to understand why some people can reduce their dose over time while others can’t stop entirely. That’s where real-world experience matters—what works for one person might not work for another, even with the same diagnosis.
Below, you’ll find practical guides on managing side effects, understanding lab results, recognizing warning signs, and making smarter choices when biologic DMARDs are part of your treatment plan. No fluff. Just what you need to stay safe, informed, and in control.