For many people living with rheumatoid arthritis (RA), the daily pain, stiffness, and swelling aren’t just inconvenient-they’re life-limiting. Before biologic DMARDs, RA was often a slow, relentless march toward joint destruction and disability. Today, that’s no longer the norm. With the right treatment, biologic DMARDs can stop the damage in its tracks and even push the disease into remission. But what does that really mean? And who benefits the most?
What Are Biologic DMARDs, and How Do They Work?
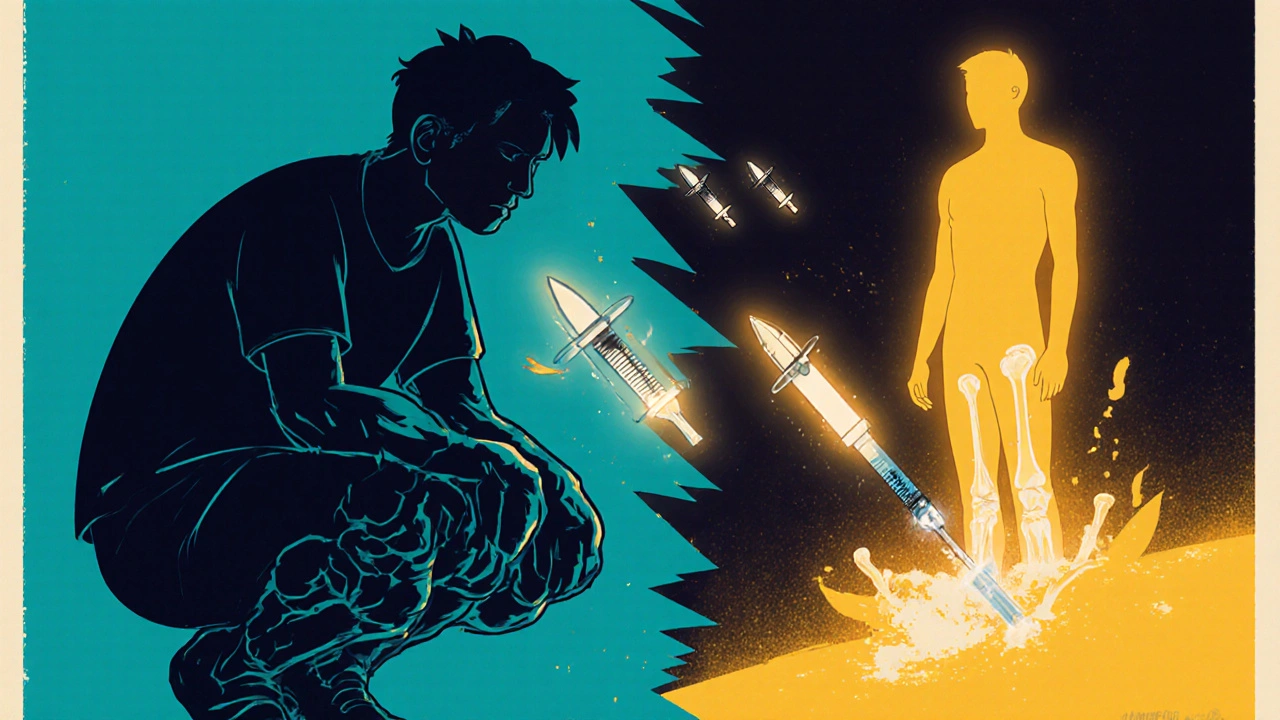
Biologic DMARDs, or biologic disease-modifying antirheumatic drugs, are targeted therapies made from living cells. Unlike older drugs like methotrexate that broadly suppress the immune system, biologics zero in on specific parts of the immune response that drive RA inflammation. Think of them as precision missiles instead of scatter shots. They block key players like tumor necrosis factor (TNF), interleukin-6 (IL-6), or T-cells that mistakenly attack your joints. The first one, etanercept (Enbrel), was approved in 1998. Since then, dozens have followed, each targeting a different piece of the inflammation puzzle. Some are injected under the skin weekly or every other week. Others require an IV infusion every few weeks. The goal isn’t just to feel better-it’s to stop the disease from eating away at your bones and cartilage.Remission Isn’t a Dream-It’s a Realistic Goal
Remission in RA doesn’t mean you’re cured. It means your disease is so well controlled that symptoms are minimal or gone, and tests show little to no active inflammation. The American College of Rheumatology defines remission using scores like DAS28, which measures joint swelling, pain, and blood markers of inflammation. If your score is low enough, you’re in remission. Here’s the key: biologic DMARDs make remission possible for far more people than older drugs ever could. Studies show that only 5-15% of RA patients on methotrexate alone reach remission. With biologics, that number jumps to 20-50%. In real-world clinics, patients who start biologics after methotrexate fails often see their pain drop by half within 3 months. One case study from 2022 described a patient with 15 years of severe RA achieving full remission in just 8 weeks after starting tocilizumab.Not All Biologics Are the Same-Here’s How They Compare
There are two main groups: TNF inhibitors and non-TNF biologics. TNF blockers like adalimumab (Humira), etanercept (Enbrel), and infliximab (Remicade) were the first wave. They work fast-many patients feel relief in days. But newer drugs targeting other pathways often do better in the long run. - TNF inhibitors: Humira, Enbrel, Remicade. Fast-acting, widely used. But up to 40% of patients don’t respond well, or lose response over time. - IL-6 blockers: Tocilizumab (Actemra). Works well for patients with high inflammation markers. Often used when TNF drugs fail. - T-cell modulators: Abatacept (Orencia). Slower to work but very safe long-term. Good for patients with infection risks. - B-cell depleters: Rituximab (Rituxan). Best for patients with specific immune signatures-like high B-cell activity in joint tissue. - JAK inhibitors: Tofacitinib, upadacitinib. Not technically biologics, but they work similarly. Taken as pills. Highly effective, but carry boxed warnings for blood clots and heart risks. A 2022 review found that non-TNF biologics and JAK inhibitors were 19% more effective than TNF inhibitors in real-world settings. Why? Because RA isn’t one disease-it’s many. What works for one person might do nothing for another.
Who Gets Biologics-and Who Doesn’t?
Guidelines are clear: methotrexate comes first. It’s cheap, well-studied, and works for many. Biologics are reserved for people who don’t respond adequately after 3-6 months on methotrexate-or those with aggressive disease from the start. But access isn’t equal. In the U.S. and Western Europe, 25-30% of RA patients get biologics. In developing countries, it’s often under 10%. Why? Cost. A year of Humira or Enbrel can run $50,000-$70,000 in the U.S. Even with insurance, copays can hit $1,000 a month. That’s why biosimilars-cheaper copies of brand-name biologics-are changing the game. By mid-2023, they made up 35% of TNF inhibitor prescriptions in the U.S., cutting out-of-pocket costs by 15-30%.The Real-World Experience: Successes and Struggles
On patient forums, the stories are mixed but mostly hopeful. Of over 1,200 people surveyed on the Arthritis Foundation’s site, 68% said biologics dramatically improved their lives. Adalimumab got the highest satisfaction rating at 4.2 out of 5. Many describe going from wheelchairs to walking again, or from missing work every week to holding down a full-time job. But it’s not all smooth sailing. About 32% report side effects. The most common: injection site redness (45%), increased infections like pneumonia or skin abscesses (30%), and the emotional toll of financial stress (25%). One Reddit user wrote: “I got my first shot on a Friday. By Monday, I had a fever and couldn’t get out of bed. It took weeks to recover.” Another big issue is secondary failure. After 12-24 months, nearly 40% of patients find their drug stops working. That’s when doctors switch to another biologic-or a JAK inhibitor. But here’s the catch: each new drug after the first tends to work less well. That’s why choosing the right first biologic matters so much.
How to Make Biologics Work for You
Getting started isn’t just about picking a drug. It’s about preparation. - Training: Most biologics are self-injected. Nurses typically teach patients in 1-2 sessions. By the end of the month, 75% of patients are managing it alone. - Monitoring: You’ll need blood tests every 2-3 months to check liver function, blood counts, and infection markers. Watch for fever, chills, or unexplained fatigue-signs you might be getting sick. - Insurance: Getting approval can take 7-14 days. Work with your rheumatologist’s office-they have specialty pharmacy teams that handle prior authorizations. - Support: Drugmakers offer patient assistance programs that can cover 40-100% of costs. Apps like ArthritisPower let you track symptoms and share data with your doctor.What’s Next? The Future of RA Treatment
The next wave is personalization. Researchers are now analyzing synovial tissue from joints to predict which drug will work best. If your joint fluid shows high B-cell activity, rituximab might be your best shot. If IL-6 is the main driver, tocilizumab wins. This isn’t science fiction-it’s happening in clinics right now. Longer-acting biologics are coming too. A twice-yearly injection of tocilizumab is in late-stage trials. That means fewer shots, fewer visits, and better adherence. And biosimilars will keep growing. By 2027, they could make up 60% of the biologic market. That’s not just good for your wallet-it’s good for the system. More people will get access to life-changing treatment.Final Thought: It’s Not About One Drug-It’s About Finding Your Path
There’s no single “best” biologic. What works for your neighbor might not work for you. The goal isn’t to try every drug until something sticks. It’s to work with your rheumatologist, understand your disease pattern, and pick the most strategic first step. Remission is possible. But it takes time, patience, and the right plan. Don’t give up if the first drug doesn’t work. Don’t skip your blood tests. Don’t let cost stop you-ask about assistance programs. RA doesn’t have to be a life sentence anymore. With the right tools, it can be a manageable condition-and for many, a quiet one.Can biologic DMARDs cure rheumatoid arthritis?
No, biologic DMARDs cannot cure rheumatoid arthritis. But they can put the disease into remission, meaning symptoms disappear and inflammation stops causing damage. Most people need to keep taking them long-term to stay in remission. Stopping the drug often leads to a flare-up.
How long does it take for biologic DMARDs to work?
TNF inhibitors like Humira or Enbrel often start working in 1-4 weeks. Non-TNF biologics like abatacept or tocilizumab may take 3-6 months to show full effects. Patience is key-don’t switch drugs too soon. Give each one at least 3 months to work before deciding it’s not right for you.
Are biosimilars as effective as brand-name biologics?
Yes. Biosimilars are highly similar to their brand-name counterparts and work just as well in most patients. Studies show no meaningful difference in effectiveness or safety. Many patients switch successfully from Humira to its biosimilar without losing control of their RA. Insurance companies often push biosimilars because they cost 15-30% less.
What are the biggest risks of biologic DMARDs?
The biggest risk is serious infections, including tuberculosis, pneumonia, and skin infections. Before starting, you’ll be screened for TB and hepatitis. Other risks include allergic reactions, injection site reactions, and, for JAK inhibitors, increased risk of blood clots and heart problems. Regular blood tests and reporting any fever or unusual fatigue are critical.
Why do some people stop responding to biologics over time?
This is called secondary non-response. Your body may start making antibodies against the drug, making it less effective. Or the disease may evolve, using a different inflammatory pathway. About 40% of patients experience this after 1-2 years. That’s why doctors plan ahead-they don’t just pick one drug and stick with it. They have backup options ready.
Can I take biologic DMARDs with methotrexate?
Yes, and many patients do. Combining methotrexate with a biologic often works better than either alone. Methotrexate can reduce the chance of your body rejecting the biologic drug. But some people can’t tolerate methotrexate due to side effects, and biologics can still work on their own. Your doctor will decide based on your health and response.
Is it safe to get vaccines while on biologic DMARDs?
Yes-but timing matters. You should get all routine vaccines (flu, pneumonia, shingles) before starting a biologic if possible. Live vaccines (like MMR or nasal flu) are not safe while on these drugs. Inactivated vaccines (like the flu shot or COVID boosters) are safe and strongly recommended. Always check with your rheumatologist before getting any vaccine.

Debanjan Banerjee
November 20, 2025 AT 11:46Biologics changed my life-no more morning stiffness that felt like my joints were glued shut. I was on methotrexate for two years with zero improvement. Started adalimumab, and within six weeks, I could hold a coffee cup without wincing. It’s not magic, but it’s the closest thing we’ve got.
Biggest hurdle? Insurance. Took three appeals and a letter from my rheumatologist just to get approved. Biosimilars are a godsend-my copay dropped from $1,200 to $400. If you’re struggling with access, don’t give up. Call your pharma’s patient assistance program. They’re more helpful than you think.
Steve Harris
November 21, 2025 AT 23:57As someone who’s been managing RA for 18 years, I’ve seen the shift from prednisone dependence to biologics. The science here is solid. But let’s be real-this isn’t just about drugs. It’s about systemic access. In rural America, getting to an infusion center twice a month is a logistical nightmare. Telehealth helps, but it doesn’t replace blood draws or joint checks.
Also, please stop calling it ‘remission’ like it’s a finish line. It’s a maintenance phase. You’re not cured-you’re just in a really good holding pattern. And that’s okay.
Michael Marrale
November 22, 2025 AT 05:39EVERYONE knows biologics are just a front for Big Pharma to sell you lifelong dependency. They’re not curing anything-they’re making you dependent on $70k/year injections while they patent the next ‘miracle drug’ every 3 years.
Have you heard about the 2017 whistleblower report? The FDA knew TNF blockers increased lymphoma risk by 400% but delayed the warning for 14 months. They’re selling you hope so they can sell you more drugs. Wake up.
Also, why do you think they banned the natural anti-inflammatories? Turmeric? Ginger? No one can patent those. It’s all about control.
David vaughan
November 23, 2025 AT 18:46Just wanted to say… I’ve been on rituximab for 18 months. It’s not perfect. I get tired. I had a mild pneumonia last winter. But I can play with my kids again. That’s worth it.
Also, if you’re scared of injections? I was too. My nurse showed me how to do it with a mirror. Now I do it while watching Netflix. It’s not fun, but it’s manageable.
And yes, the cost is insane. But my drug company gave me a $500/month voucher. Just ask. They want you to stay on it.
Don’t let fear stop you. You’re not alone.
Cooper Long
November 25, 2025 AT 10:35Biologics represent a paradigm shift in rheumatology. The transition from non-specific immunosuppression to targeted molecular intervention marks a significant advancement in chronic disease management. The data supporting remission rates is robust and reproducible across multiple cohorts.
Logan Romine
November 26, 2025 AT 20:31So let me get this straight… we spend $70,000 a year to turn RA into a chronic condition you have to manage with a syringe… instead of just accepting that your body’s broken?
Meanwhile, my grandma in 1972 took aspirin, sat in a rocking chair, and lived to 92. Maybe we’re overengineering suffering?
Also, why do we call it ‘remission’ and not ‘temporary ceasefire’? Sounds like PR spin. 🤷♂️
Franck Emma
November 27, 2025 AT 05:27I cried the first time I walked to my mailbox without pain.
Then I got a $1,200 bill.
Then my insurance denied my refill.
Then I got shingles.
Now I’m on a different biologic.
And I’m still here.
Don’t tell me this isn’t a miracle. It’s a miracle that costs more than my car.
Eliza Oakes
November 28, 2025 AT 18:10Okay but have you considered that RA isn’t even an autoimmune disease? It’s just your body’s way of telling you you’ve been eating too much gluten and sitting on your butt all day?
I read this one blog that said 90% of RA cases are cured by intermittent fasting and cold showers. Biologics? That’s just Big Pharma’s way of keeping you docile while they monetize your pain.
Also, why do you think they don’t talk about the 1987 study where patients got better after drinking apple cider vinegar? 🤔
Someone’s hiding something. I know it.
Shawn Sakura
November 29, 2025 AT 21:09Just wanted to say… you’re not broken. You’re not weak. You’re fighting a war no one else sees.
I started on Enbrel last year. I was skeptical. I thought it was just another expensive placebo. But after 3 months? I could hug my wife without flinching.
Yeah, the shots suck. Yeah, the insurance drama is insane. But you’re worth it.
And if you’re scared to start? Just take it one day at a time. One injection. One breath. One step.
You’ve got this. 💪❤️
Swati Jain
December 1, 2025 AT 16:28Biologics? More like bioweapons with a price tag. 😏
Let’s be real-RA isn’t a disease, it’s a symptom of modern life. Sitting. Stress. Sugar. Glyphosate. Biologics treat the symptom, not the cause. Meanwhile, your doctor’s too busy to ask if you’ve slept more than 4 hours this week.
But hey, if you want to drop $70K and get a fancy injection schedule? Go for it. Just don’t call it ‘remission’-call it ‘chemical sedation.’
Meanwhile, I’m doing yoga, eating turmeric, and laughing at the system. 😌
Florian Moser
December 3, 2025 AT 06:49For anyone considering biologics: give it time. Don’t quit after 4 weeks. It’s not a fast fix. It’s a slow rebuild.
My first drug didn’t work. Second one gave me a rash. Third one? Tocilizumab. Took 12 weeks. But now? I’m hiking. I’m working full-time. I’m sleeping through the night.
It’s not perfect. But it’s better than a wheelchair.
And if cost is an issue-ask. Always ask. There are programs. People want you to succeed.
jim cerqua
December 4, 2025 AT 18:19Let’s talk about the elephant in the room: 40% of people stop responding? That’s not a treatment-it’s a revolving door.
And what happens when you’ve tried all 6 biologics and JAK inhibitors and still flare? Then what? You’re just… out of options?
They sell you hope. Then they sell you the next hope. Then they sell you the next hope. And when the hope runs out? You’re left with a mountain of debt and a body that still hurts.
This system is rigged.
Donald Frantz
December 6, 2025 AT 13:05Interesting breakdown. But you didn’t mention the role of gut microbiome in biologic response. Emerging data shows patients with higher microbial diversity respond better to TNF inhibitors. Could be a confounder in real-world outcomes.
Also, why is there no data on long-term cancer risk beyond 5 years? Most trials end at 24 months. That’s not enough.
And biosimilars-while cost-effective-still lack head-to-head data with original biologics in seronegative RA. We’re assuming equivalence. That’s risky.
Sammy Williams
December 7, 2025 AT 20:31I got my first shot last week. Still scared. Still tired. But I held my nephew today. That’s all that matters.