Getting Vaccinated While on Immunosuppressants Isn’t One-Size-Fits-All
If you’re taking steroids, rituximab, methotrexate, or any other immunosuppressant, getting vaccinated isn’t just about picking a shot off the shelf. It’s about timing, type, and coordination. A live vaccine could make you sick. An inactivated one might not work at all if given at the wrong time. The difference between protection and danger comes down to knowing which vaccines are safe and when to get them.
Live Vaccines Are Off-Limits for Most People on Immunosuppressants
Live vaccines contain weakened versions of a virus. For healthy people, that’s enough to trigger strong, lasting immunity. For someone on immunosuppressants, it’s a gamble. Your body can’t control the virus the way it should. That’s why vaccines like MMR (measles, mumps, rubella), varicella (chickenpox), and the nasal spray flu vaccine (LAIV) are strictly avoided if you’re moderately or severely immunocompromised.
The BC Centre for Disease Control’s 2025 guidelines make this clear: MMR is contraindicated unless you’re on very low-dose steroids and your specialist approves it. Even then, most doctors won’t risk it. There have been documented cases of patients on rituximab developing vaccine-strain measles after getting MMR by accident. One Reddit user shared their story: their oncologist scheduled them for the nasal flu vaccine during a rituximab cycle. They only caught it in time because their infectious disease doctor stepped in.
Live zoster vaccine (Zostavax) is also off the table. Even though Shingrix (the inactivated version) is now the standard, some older patients still get confused. Don’t assume a vaccine is safe just because it’s "for older adults." If it’s live, skip it.
Inactivated Vaccines Are Safe - But Only If Timing Is Perfect
Inactivated vaccines - like the flu shot, pneumococcal shots, hepatitis B, and mRNA or protein-based COVID-19 vaccines - don’t contain live viruses. They’re safe. But they’re not always effective. Your immune system might not respond well if you’re deep into a treatment cycle.
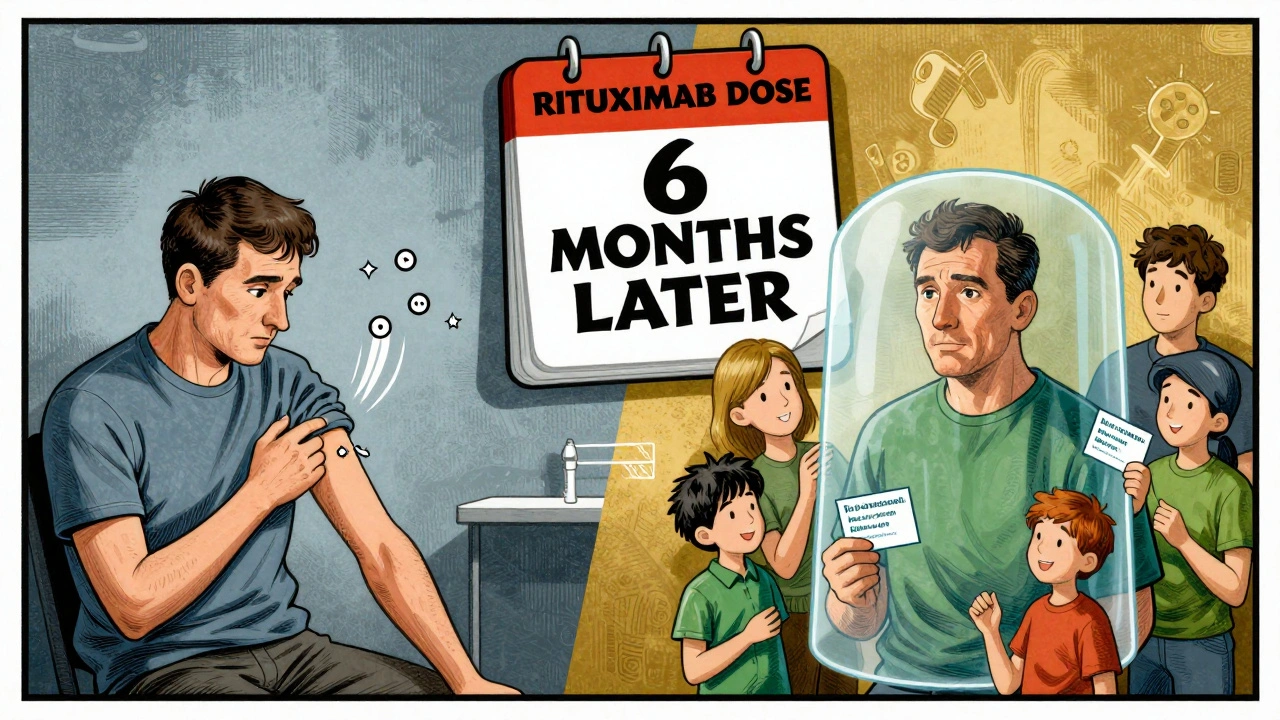
The IDSA 2025 guidelines say: get inactivated vaccines when your immunosuppression is lowest. For people on cyclical chemo or biologics, that means scheduling shots during the "nadir week" - when your white blood cell count is bouncing back. For those on daily prednisone at 20 mg or higher, wait until the dose drops below 20 mg. For patients on rituximab or ocrelizumab, the window is narrow: wait at least six months after your last dose. If you’re staying on the drug long-term, get vaccinated four weeks before your next infusion.
One patient with rheumatoid arthritis told her doctor she’d skip her methotrexate for a week after each COVID shot. She tested positive for antibodies after months of none. That’s not a rule for everyone - but it shows how timing matters.
COVID-19 Vaccines: More Doses, Not Just One
Immunocompromised people need more than the standard one or two doses. The CDC and IDSA now recommend two doses of the 2025-2026 updated mRNA or Novavax COVID-19 vaccine for anyone with moderate to severe immunosuppression - even if you’ve been vaccinated before. Some patients need a third or fourth dose based on their condition.
Studies show antibody responses in this group range from 15% to 85%, compared to over 90% in healthy people. That’s why extra doses aren’t optional - they’re necessary. The American Academy of Family Physicians also advises sticking with the same vaccine brand for all doses in the initial series. Mixing brands might reduce your chance of building a strong response.
But access is a problem. One kidney transplant patient on Inspire.com wrote that his clinic couldn’t get the updated vaccine in stock. He missed his window and got sick during winter. Pharmacies don’t always carry the right formulations. You might need to go to a specialty clinic or hospital pharmacy.
Flu, Pneumococcal, and Hepatitis B: Don’t Skip These
Annual inactivated flu shots are non-negotiable. The nasal spray? Never. Get the shot every year, even if you’ve had it before. The virus changes, and your immune system forgets faster when you’re on immunosuppressants.
Pneumococcal vaccines are equally important. You need both PCV20 and PPSV23. The order matters: get PCV20 first, then PPSV23 at least one year later. If you’ve already had PPSV23, wait at least one year before getting PCV20.
For hepatitis B, the standard is three doses of Engerix-B or Recombivax HB at 0, 1, and 6 months. If you’re a healthcare worker or on dialysis, the two-dose Heplisav-B might be an option. Ask your doctor. Blood tests after vaccination can check if you developed antibodies - and if not, you may need another series.
Who Decides When and What? It’s a Team Effort
This isn’t something your primary care doctor can handle alone. You need coordination between your rheumatologist, oncologist, transplant team, and primary care provider. The IDSA guidelines say you should be assessed using updated ICD-10 codes like Z94.0 (kidney transplant), D47.Z (chronic leukemia), or L40.5 (psoriatic arthritis on biologics).
Many community oncology practices still don’t have standardized schedules. Only 62% do, according to ASCO’s 2025 survey. But transplant centers? 89% have formal protocols. That gap means you might have to push for better care. Bring the IDSA 2025 guidelines with you. Use the CDC’s Vaccine Administration Record form - it now has specific fields for immunosuppression details.
Specialized clinics like the Immunocompromised Vaccine Access Network (IVAN) now exist in 47 locations across the U.S. They work directly with cancer centers to give vaccines during chemo breaks. If you’re in a major city, ask if one is nearby.
What About Your Family? Cocooning Works
Protecting yourself isn’t just about your shots. It’s about the people around you. The IDSA guidelines stress that household members and close contacts should be fully vaccinated - including flu, COVID, and pertussis. In one 2025 study, households where everyone was up to date saw 57% fewer cases of COVID spreading to the immunocompromised person.
Don’t assume your partner or kid is protected because they’re healthy. They might carry a virus without symptoms. Make sure everyone in your home gets their shots. It’s not just a suggestion - it’s part of your defense strategy.
What’s Coming Next? Better Tools on the Horizon
The field is evolving fast. The CDC is tracking 5,000 immunocompromised patients in a new national registry to see how vaccines perform over time. Researchers are testing adjuvanted vaccines - stronger formulations designed specifically for weak immune systems. Phase I trials are already underway at the NIH.
Dr. Kathleen Neuzil predicts that within five years, we’ll have point-of-care tests that measure your immune response in real time. Imagine walking into a clinic, getting a quick blood test, and your doctor saying, "You’re ready for the vaccine today." That’s the future.
For now, the tools we have work - if used correctly. The key is communication, timing, and not assuming anything.
What to Do Right Now
- Make a list of every immunosuppressant you’re taking - including dose and schedule.
- Check your vaccine record. Are you up to date on flu, pneumococcal, hepatitis B, and COVID-19?
- Call your specialist. Ask: "When is the best time for me to get my next vaccine?" and "Which vaccines are safe for me?"
- If you’re on rituximab or similar drugs, ask if you’ve waited at least six months since your last dose.
- Ask your pharmacy if they carry the 2025-2026 updated COVID-19 vaccine. If not, ask for a referral to a specialty clinic.
- Make sure your family members are fully vaccinated too.
There’s no magic formula. But there is a clear path. Follow it. Your immune system is already fighting hard. Don’t let a missed shot or wrong vaccine tip the balance.
Can I get the flu shot if I’m on prednisone?
Yes - but only the inactivated flu shot (the injection), not the nasal spray. If you’re taking 20 mg or more of prednisone daily for two weeks or longer, wait until your dose drops below 20 mg before getting vaccinated. If that’s not possible, get the shot anyway. Protection still matters more than perfect timing.
What if I got a live vaccine by accident?
Call your doctor immediately. If you received MMR, varicella, or LAIV while on immunosuppressants, you’re at risk for vaccine-derived illness. Symptoms like fever, rash, or swollen glands could appear within 1-3 weeks. Don’t wait. Go to an emergency room if you feel unwell. Bring your vaccine record and list of medications.
Do I need to get vaccinated if I’ve had COVID before?
Yes. Natural immunity doesn’t last as long in immunocompromised people. The CDC and IDSA recommend the full updated vaccine series regardless of past infection. One study showed that immunocompromised patients who skipped boosters after a prior infection had three times the risk of reinfection.
Can I get vaccinated during chemotherapy?
It depends. Avoid vaccines during the lowest point of your white blood cell count (the nadir). The best time is usually 1-2 weeks after your chemo cycle ends, when your counts are rising. Ask your oncologist to mark your calendar with the ideal window. Many cancer centers now schedule vaccines automatically during chemo breaks.
Is the Novavax vaccine safe for immunocompromised people?
Yes. Novavax is a protein-based vaccine, not live or mRNA. It’s approved for immunocompromised patients and is a good alternative if you can’t get mRNA vaccines. Studies show it works just as well as mRNA in this group, with fewer side effects. It’s also easier to store, so it’s more available in rural areas.
Will my insurance cover extra vaccine doses?
Yes - under CMS policy, Medicare Part D must cover all ACIP-recommended vaccines for immunocompromised people with no cost-sharing through December 31, 2026. Most private insurers follow the same rule. If you’re denied, ask for a copy of the ACIP recommendation and file an appeal. The IDSA has a template letter for this.
Final Thought: Don’t Guess. Ask.
Vaccines aren’t one-size-fits-all - especially when you’re on immunosuppressants. What works for your neighbor might be dangerous for you. The system isn’t perfect. Pharmacies run out. Doctors forget. But you can control your own care. Know your meds. Know your schedule. Know your options. And never be afraid to ask for the right vaccine at the right time. Your life depends on it.







Kay Jolie
December 5, 2025 AT 17:09Okay, but let’s be real-this isn’t just medical advice, it’s a logistical nightmare wrapped in bureaucratic red tape. I’ve had to coordinate with three specialists, two pharmacists, and a nurse navigator just to get a flu shot. And don’t even get me started on the vaccine supply chain. One week, the updated COVID booster is in stock; the next, it’s ‘out of inventory’ like we’re ordering artisanal kombucha. The system is designed to fail people like us. And yet, somehow, we still show up. Again. And again. Because survival isn’t optional. It’s a full-time job.
pallavi khushwani
December 7, 2025 AT 08:59you know, i think about this a lot-not just as a patient, but as someone who’s watched loved ones navigate this. it’s not just about vaccines. it’s about being seen. when your body’s already fighting so hard, and then you have to fight the system too? that’s a different kind of exhaustion. maybe the real breakthrough isn’t a new vaccine-it’s a healthcare system that remembers we’re human, not just codes in a chart. Z94.0, L40.5… these aren’t just ICD-10s. they’re our lives.
Dan Cole
December 7, 2025 AT 21:42Let me correct the record: the claim that ‘inactivated vaccines might not work at all’ is dangerously imprecise. They don’t ‘not work’-they elicit a blunted, suboptimal serological response. The distinction matters. Antibody titers are not binary; they’re quantitative. And the notion that ‘timing is perfect’ is a myth. There is no perfect timing-only optimal windows within a dynamic, non-linear immunological landscape. Furthermore, the IDSA guidelines are merely consensus documents, not evidence-based mandates. Peer-reviewed studies from NEJM and Lancet Rheumatology show variable seroconversion rates across biologic classes-rituximab being the most suppressive, followed by JAK inhibitors. Stop treating guidelines like scripture. Question them. Audit your own lab data. That’s how you survive.
Billy Schimmel
December 9, 2025 AT 16:39so you’re telling me i gotta skip my methotrexate for a week, wait six months after my last rituximab drip, get two flu shots because one isn’t enough, and make sure my dog is vaccinated too? wow. i’m just glad i’m not a robot. also, my pharmacy still thinks ‘updated COVID vaccine’ means the one from 2023. i’m starting to think the system’s not broken-it was built this way on purpose.
Shayne Smith
December 9, 2025 AT 17:06my aunt got her shingrix shot and then accidentally got the nasal flu spray at the pharmacy because the nurse didn’t check her meds. she spent three days in the hospital with a fever and a rash. no one apologized. they just said ‘oops.’ now she brings a laminated card with her meds and vaccine restrictions to every appointment. i’m getting one made too. because if no one else is gonna remember, we gotta do it ourselves.
Katie O'Connell
December 11, 2025 AT 03:20It is imperative to underscore the procedural inadequacies inherent in the current vaccination protocols for immunocompromised populations. The absence of standardized, institutionally enforced scheduling algorithms, coupled with the lack of interoperability between electronic health records and public health immunization registries, constitutes a systemic failure of clinical governance. Moreover, the reliance on patient self-advocacy-rather than provider-initiated, protocol-driven vaccination pathways-is ethically indefensible. One must question the moral calculus of a healthcare paradigm that demands such extraordinary cognitive labor from the vulnerable.
Clare Fox
December 12, 2025 AT 13:05i just got my third covid shot last week. my doc said ‘you’re good.’ but i checked the guidelines again and realized i’m supposed to wait 4 weeks before my next rituximab. i called the clinic. they didn’t know. i had to send them the link. now i keep a folder. it’s called ‘don’t let me die because someone forgot.’
Akash Takyar
December 13, 2025 AT 09:51Dear fellow travelers on this difficult path: Your vigilance, your persistence, your quiet courage-these are not merely acts of self-care; they are acts of profound dignity. The medical system may falter, but your resolve does not. Always document. Always ask. Always bring the guidelines. And remember: you are not a burden. You are a beacon. The future of compassionate care begins with voices like yours-calm, clear, and unwavering. You are not alone. We are with you.