Rheumatoid Arthritis: Causes, Management, and What You Need to Know
When your body turns on itself, that’s rheumatoid arthritis, a chronic autoimmune disease where the immune system mistakenly attacks the lining of your joints. Also known as RA, it doesn’t just hurt—it can wear down bone, damage organs, and make simple tasks like opening a jar or walking up stairs feel impossible. Unlike regular arthritis from wear and tear, rheumatoid arthritis is systemic. It doesn’t stop at the knees or hands. It can affect your lungs, heart, eyes, and even your skin. And it’s not just old people—it often hits between ages 30 and 60, and women are three times more likely to get it than men.
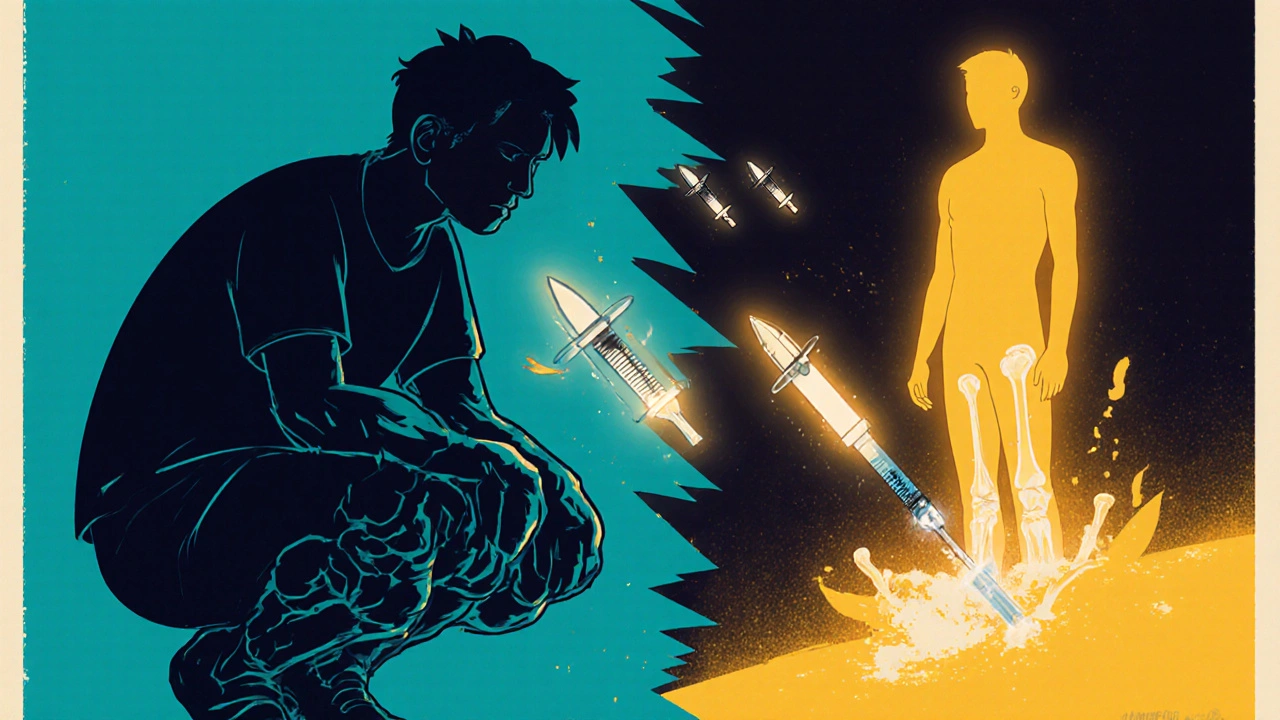
What makes it tricky is how closely it ties to other health issues you might be managing. If you’re on immunosuppressive therapy, drugs that quiet down your overactive immune system to stop joint damage, you’re walking a tightrope. These meds—like methotrexate, biologics, or JAK inhibitors—help control RA, but they also lower your body’s defenses. That means you’re more vulnerable to infections, and some can even mess with your liver or blood counts. That’s why regular lab tests, like blood counts, liver enzymes, and kidney function checks aren’t optional. They’re your early warning system. And if you’re also taking other meds—for blood pressure, diabetes, or even sleep—those can interact in ways you won’t see coming. Your medical history isn’t just background info; it’s the map that tells your doctor what drugs are safe for you.
There’s no cure, but there’s a lot you can do to take back control. Diet doesn’t fix RA, but some foods reduce inflammation and others make it worse. Sleep matters—not just because you’re tired, but because poor sleep fuels inflammation. And sticking to your meds? That’s the biggest game-changer. Skipping doses or stopping because you feel better is one of the fastest ways to see your joints start breaking down again. The good news? Modern treatments have come a long way. Many people with RA now live full, active lives. It’s not about waiting for the pain to go away. It’s about managing it before it manages you.
Below, you’ll find real, practical guides on how RA connects to the drugs you take, the tests you need, and the hidden risks that come with long-term treatment. No fluff. No guesswork. Just what works—and what to watch out for.