Potassium Safety Calculator
Personal Information
Daily Food Intake
Your Daily Potassium Summary
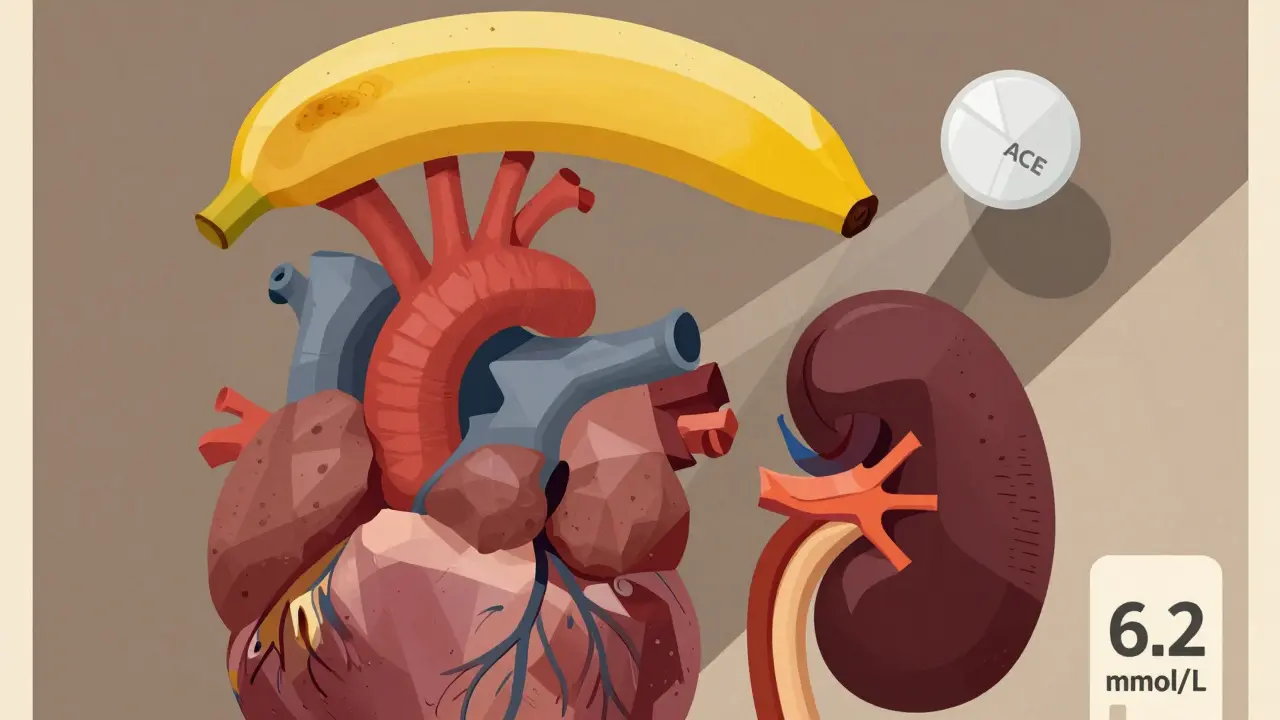
When you’re on an ACE inhibitor-like lisinopril, enalapril, or ramipril-for high blood pressure, heart failure, or kidney disease, you’re getting real protection for your heart and kidneys. But there’s a quiet danger hiding in plain sight: your food. Too much potassium, especially from healthy fruits and veggies, can push your blood potassium levels into dangerous territory. This isn’t theoretical. About 1 in 5 people on ACE inhibitors develop hyperkalemia, and for those with kidney problems, the risk is even higher.
Why ACE Inhibitors Raise Potassium Levels
ACE inhibitors work by blocking a system in your body called RAAS-the renin-angiotensin-aldosterone system. This system normally helps control blood pressure by releasing aldosterone, a hormone that tells your kidneys to get rid of extra potassium. When ACE inhibitors shut down aldosterone production, your kidneys hold onto potassium instead of flushing it out. Studies show aldosterone drops by 40-60% within a day of starting the medication. That means potassium clearance drops by 25-35%. Your body doesn’t know how to get rid of it anymore.This isn’t just about the drug. It’s about your kidneys. If your eGFR (a measure of kidney function) is below 60 mL/min/1.73m², your risk of hyperkalemia jumps 3.2 times. If you have diabetes, especially with protein in your urine, your risk goes up another 47%. Combine that with older age, heart failure, or another medication like spironolactone or trimethoprim, and you’re in high-risk territory.
Which Foods Are the Biggest Culprits?
You don’t need to give up healthy eating. But you do need to know which foods pack a potassium punch. Many people think they’re doing the right thing by eating more fruits and vegetables-until their blood test shows potassium at 6.2 mmol/L. That’s life-threatening.Here are the top offenders, with potassium content per typical serving:
- One medium banana: 422 mg
- One medium orange: 237 mg
- One baked potato (with skin): 926 mg
- One cup cooked spinach: 839 mg
- One cup avocado: 708 mg
- One medium tomato: 292 mg
- One sweet potato (baked): 542 mg
- One cup coconut water: 1,150 mg
- One cup cooked lentils: 731 mg
Even foods labeled "healthy" can be dangerous. Protein powders, salt substitutes (which often contain potassium chloride), and certain energy drinks are hidden sources. A Reddit user in Perth shared how they spiked their potassium after drinking 16 oz of coconut water daily thinking it was "better than sports drinks." That’s over 1,100 mg in one drink-more than half the daily limit for someone with kidney disease.
How Much Potassium Is Safe?
There’s no one-size-fits-all number. The National Kidney Foundation says if your eGFR is below 45 mL/min/1.73m², aim for under 2,000 mg of potassium per day. If your kidneys are working better (eGFR above 60), you might be able to tolerate up to 3,000 mg. But if you’re on an ACE inhibitor and your potassium has ever been above 5.0 mmol/L, stick to the lower end.Most people in Australia eat around 3,000-4,000 mg daily. That’s fine if your kidneys are healthy. But if you’re on an ACE inhibitor and have kidney disease, you’re eating nearly double what’s safe. That’s why diet changes aren’t optional-they’re essential.
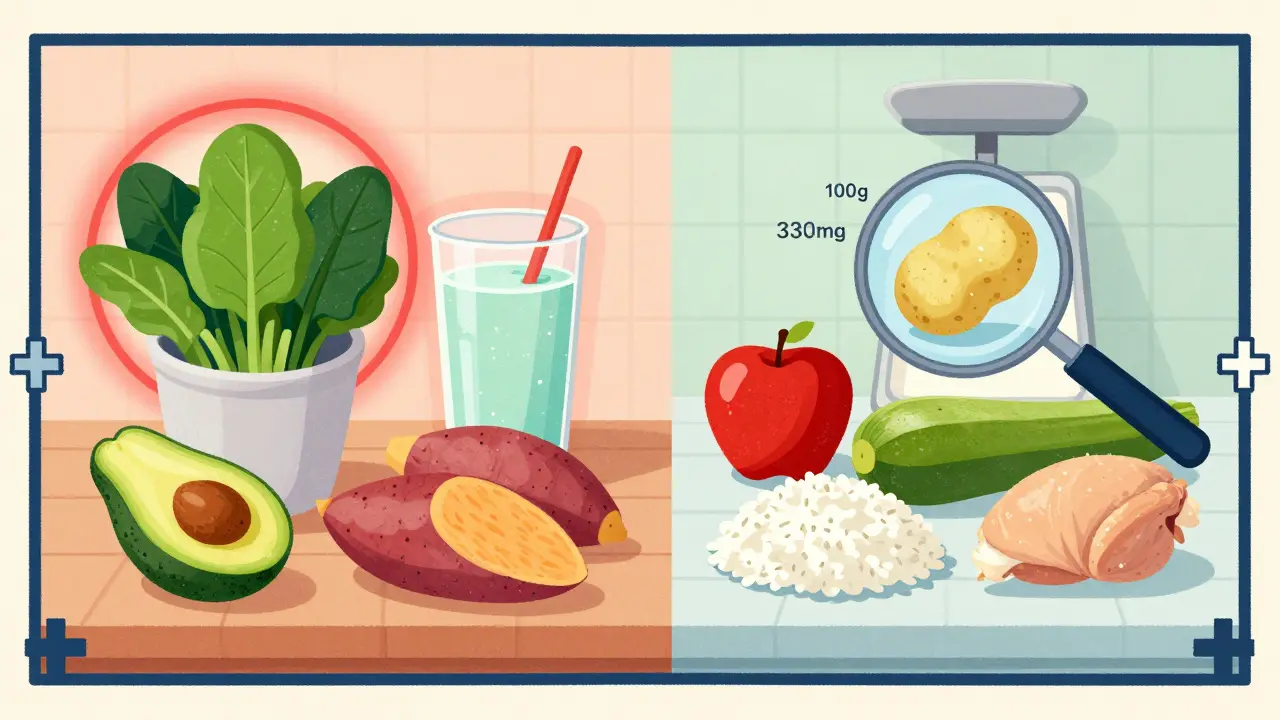
What You Can Still Eat
You don’t have to live on plain rice and boiled chicken. There are low-potassium alternatives that still taste good:- Apples, berries, grapes, pineapple (instead of bananas, oranges, melons)
- Cabbage, green beans, zucchini, cauliflower (instead of spinach, potatoes, tomatoes)
- White rice, pasta, noodles (instead of whole grains or quinoa)
- White bread (instead of whole wheat)
- Chicken, turkey, fish (instead of processed meats with added potassium)
Even better: leach your vegetables. Boil potatoes, carrots, or beetroot in plenty of water, then drain and rinse them. This can cut potassium by 50% or more. It’s a simple trick used by renal dietitians across Australia and the U.S.
Monitoring and Testing Are Non-Negotiable
Your doctor should check your potassium and kidney function before you start an ACE inhibitor. Then again 7-14 days after starting, after any dose change, and every 4 months after that. If your creatinine rises by more than 30% or your potassium climbs above 5.5 mmol/L, your dose may need to be lowered-or switched.Don’t wait for symptoms. Hyperkalemia often has none. When it does, you might feel weak, dizzy, or notice your heart skipping beats. But by then, it’s already dangerous. Regular blood tests are your safety net.
What About New Medications?
There’s good news: new drugs called potassium binders-like patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma)-can help. These pills grab excess potassium in your gut and flush it out in your stool. Clinical trials show they reduce the chance of stopping your ACE inhibitor due to high potassium by 41%. They’re not cheap, and they’re not for everyone. But if you’re at high risk and your doctor says you need to stay on your ACE inhibitor, they’re a game-changer.And research is moving forward. A new drug called KBP-5074, still in trials, is designed to protect the heart without raising potassium. Early results show it kept potassium levels normal in 82% of patients with kidney disease-compared to just 54% on placebo.
Real-World Tips That Work
Most people struggle because they don’t know what’s high in potassium. A 2022 study found 68% of patients couldn’t name three high-potassium foods. Here’s how to fix that:- Ask your doctor for a laminated food chart showing potassium levels. Keep it on your fridge.
- Download a free app like "Renal Diet Helper"-it scans barcodes and tracks potassium intake.
- See a renal dietitian. The Kidney Education Evaluation Program found that patients who got in-person counseling were 42% more likely to stick to their limits than those who only got written advice.
- Never take salt substitutes unless your doctor says yes. Many contain potassium chloride and can spike your levels fast.
- Read labels on protein powders, energy drinks, and bottled soups. Potassium is often added as a preservative or flavor enhancer.
One patient in Perth told me he started using a kitchen scale to weigh his portions. He’d always assumed a "small" potato was safe. Turns out, even a 100-gram potato has 330 mg of potassium. When he started measuring, his levels dropped from 5.8 to 4.9 in six weeks.
The Bottom Line
ACE inhibitors save lives. But they can’t do that if you stop taking them because your potassium got too high. The key isn’t fear-it’s awareness. You can still eat well, feel good, and protect your heart. You just need to know which foods to limit, how to test regularly, and when to ask for help.Don’t let a healthy diet become a hidden danger. Talk to your doctor. Get tested. Learn your numbers. And if you’re unsure about a food-look it up. Your heart will thank you.
Can I still eat bananas if I’m on an ACE inhibitor?
If your kidney function is normal and your potassium levels are stable, one banana a week might be fine. But if you have kidney disease, diabetes, or your potassium has ever been above 5.0 mmol/L, avoid bananas. A single medium banana has 422 mg of potassium-more than 20% of your daily limit if you’re on a 2,000 mg restriction. Try apples, grapes, or berries instead.
How often should I get my potassium checked on ACE inhibitors?
Before starting the medication, get a baseline blood test. Then check again 7-14 days after starting, after any dose increase, and every 4 months after that. If you have kidney disease or diabetes, your doctor may want to check every 2-3 months. Don’t skip these tests-even if you feel fine.
Is coconut water safe on ACE inhibitors?
No, it’s not safe for most people on ACE inhibitors, especially with kidney disease. One cup (240 mL) of coconut water contains about 600 mg of potassium. A full 16 oz bottle has over 1,150 mg-nearly half your daily limit. It’s marketed as a "natural electrolyte drink," but for you, it’s a potassium bomb. Stick to water, herbal tea, or low-potassium sports drinks.
Can I use salt substitutes if I’m on an ACE inhibitor?
Avoid them unless your doctor specifically says yes. Most salt substitutes contain potassium chloride instead of sodium chloride. That means you’re replacing one problem (high blood pressure) with another (dangerously high potassium). Even a teaspoon can add 800-1,000 mg of potassium. That’s enough to push your levels into danger zone.
What should I do if I accidentally eat too much potassium?
If you eat a large amount of high-potassium food-like a whole baked potato, a large avocado, or a bottle of coconut water-don’t panic. But do call your doctor or pharmacist. They may want to check your potassium level sooner than scheduled. Don’t wait for symptoms. In most cases, one slip won’t cause harm if your kidneys are still working well. But repeated mistakes can. Track what you eat and be honest with your care team.


Hilary Miller
January 21, 2026 AT 14:59Just switched to lisinopril last month and was terrified about giving up my bananas-turns out apples and grapes are fine. My cardiologist gave me a little chart and I stuck it on the fridge. Life’s easier when you know what’s safe.
Jasmine Bryant
January 23, 2026 AT 11:04i read this and thought ‘wait so my daily avocado toast is a problem?’ 😅 i had no idea. i’ve been eating one every morning for years thinking it was ‘heart healthy.’ now im scared to even look at my kitchen. maybe i should start weighing stuff like that guy in perth…
Malik Ronquillo
January 24, 2026 AT 22:47stop scaring people with food. you dont need to be paranoid about potassium. my grandpa was on ace inhibitors for 15 years and ate bananas every day. he lived to 92. stop turning healthy food into a threat
Brenda King
January 25, 2026 AT 22:08Leaching veggies is a game-changer. I boil my potatoes like my grandma taught me-two changes of water, rinse under cold, then roast. Cut potassium by half and still tastes amazing. 🙌
Liberty C
January 27, 2026 AT 00:18Of course you’re supposed to avoid coconut water. It’s marketed by wellness influencers who’ve never seen a nephrology textbook. The same people who think ‘detox teas’ cure diabetes. If you’re on an ACE inhibitor and drinking coconut water, you’re not ‘health-conscious’-you’re a walking electrolyte time bomb. Wake up.
Margaret Khaemba
January 27, 2026 AT 07:41Does anyone know if canned tomatoes are lower in potassium than fresh? I love tomato sauce but don’t want to risk it. Also-any apps you guys recommend besides Renal Diet Helper? I’m trying to keep track without going crazy.
Chiraghuddin Qureshi
January 28, 2026 AT 21:04bro i just use the ‘MyFitnessPal’ app and filter by potassium. it’s not perfect but it gets the job done. and yes, canned tomatoes are better-drain and rinse them, potassium drops like 30%. 🍅✌️
shivani acharya
January 29, 2026 AT 12:35they don’t want you to know this but the pharmaceutical companies love it when you stop eating potassium-rich food because then you need more drugs. potassium binders cost $1,200 a month. why not just tell you to eat less spinach? it’s not about your health-it’s about profit. and don’t get me started on how they pushed ACE inhibitors in the first place…
Patrick Roth
January 30, 2026 AT 21:21Actually, the 2,000 mg limit is outdated. The FDA says healthy adults need 4,700 mg. If your kidneys can’t handle it, maybe you shouldn’t be on ACE inhibitors at all. This article is fear-mongering disguised as medicine. I’ve seen patients get worse because they starved themselves of nutrients.
Oren Prettyman
February 1, 2026 AT 13:02It is imperative to emphasize, with the utmost seriousness, that the dietary recommendations outlined herein are not merely advisory, but constitute a non-negotiable clinical imperative for patients exhibiting diminished renal function, particularly those concurrently administered pharmacologic agents which impede aldosterone-mediated potassium excretion. Failure to adhere to the prescribed potassium restriction may precipitate life-threatening arrhythmias, the incidence of which is statistically elevated in this population. One must, therefore, exercise extreme diligence in the selection and preparation of dietary components, and consult with a certified renal dietitian without delay.