Stopping an antidepressant isn’t as simple as just skipping a pill. For many people, the body reacts in ways that feel terrifyingly real-dizziness, electric shocks in the head, nausea, insomnia, and overwhelming anxiety. These aren’t signs of relapse. They’re not weakness. They’re antidepressant discontinuation syndrome, a well-documented physical withdrawal reaction that happens when the brain and nervous system have adapted to the presence of the drug and suddenly lose it.
Why This Isn’t Addiction-But Still Needs Care
Antidepressants don’t cause addiction the way opioids or benzodiazepines do. You won’t crave them for a high. You won’t use them to escape reality. But your body still adjusts. Over weeks or months, your brain changes how it produces and uses serotonin, norepinephrine, and sometimes dopamine. When you stop suddenly, those systems are thrown off balance. That’s not psychological dependence. That’s neurochemical adaptation. And when it happens, your body lets you know. The term "discontinuation syndrome" was pushed by pharmaceutical companies in the 1990s to avoid the stigma of "withdrawal." But experts like Dr. David Healy argue it’s misleading. What we’re seeing is a classic withdrawal syndrome-just one that doesn’t involve cravings or compulsive use. The symptoms are real, measurable, and often under-recognized. Studies show nearly 4 out of 10 people who stop antidepressants abruptly end up misdiagnosed-sometimes told they’re having a panic attack, a virus, or a return of depression.What the Symptoms Actually Look Like (The FINISH Mnemonic)
Doctors use the mnemonic FINISH to remember the core symptoms:- Flu-like: Fatigue, muscle aches, chills, sweating, headaches, diarrhea
- Insoma: Trouble falling or staying asleep, vivid dreams, nightmares
- Nausea: Feeling sick to your stomach, vomiting, loss of appetite
- Imbalance: Dizziness, vertigo, unsteady walking, feeling off-balance
- Sensory: "Brain zaps"-sudden, brief electric shock sensations in the head, especially when moving your eyes. Tingling, numbness, ringing in the ears
- Hyperarousal: Anxiety, irritability, agitation, panic, feeling on edge
- 78% report fatigue
- 65% have insomnia
- 59% get nausea
- 63% experience "brain zaps"
Not All Antidepressants Are the Same-Half-Life Matters
The severity of withdrawal depends heavily on how long the drug stays in your system. That’s called its half-life.- Short half-life (1-12 hours): Paroxetine (Paxil), venlafaxine (Effexor), and desvenlafaxine (Pristiq). These cause the worst symptoms. People have reported brain zaps within hours of missing a dose. Venlafaxine users report 47% experience significant withdrawal.
- Medium half-life (1-3 days): Sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro). Symptoms usually start within 2-3 days. Moderate severity.
- Long half-life (4-6 days): Fluoxetine (Prozac). Because it lingers in the body, many people don’t even notice withdrawal. Some doctors use it to help others taper off shorter-acting drugs.
Tricyclics and MAOIs: The High-Risk Group
Not all antidepressants are SSRIs or SNRIs. Tricyclics (TCAs) like amitriptyline or nortriptyline can cause movement problems when stopped: stiff muscles, tremors, balance issues that mimic Parkinson’s. These are often mistaken for neurological disease. MAOIs (like phenelzine or tranylcypromine) are the most dangerous to quit cold turkey. Withdrawal can include:- Severe agitation
- Catatonia (unresponsiveness)
- Psychotic symptoms
- Myoclonus (sudden muscle jerks)
- Cognitive shutdown
How Long Does It Last? The Myth of the Two-Week Rule
Most medical guides say symptoms last 1-2 weeks. That’s true for many. But it’s not the full story. A 2022 study in the Journal of Clinical Psychiatry found that 18.7% of people who stopped SSRIs had symptoms lasting more than three months. The Surviving Antidepressants online community-home to over 15,000 people-reports that 73% experienced symptoms longer than two weeks. One in four say they lasted over six months. "Protracted withdrawal" is now recognized in updated guidelines from the Royal College of Psychiatrists. Some people have brain zaps, dizziness, or anxiety for over a year. This doesn’t mean the medication didn’t work. It means the nervous system took longer to reset. The good news? Symptoms almost always improve with time. And if you restart the original antidepressant-even just a tiny dose-symptoms usually vanish within 72 hours. That’s the key test: if it gets better fast after restarting, it’s withdrawal. If it doesn’t, it might be relapse.How to Stop Safely: The Only Proven Method
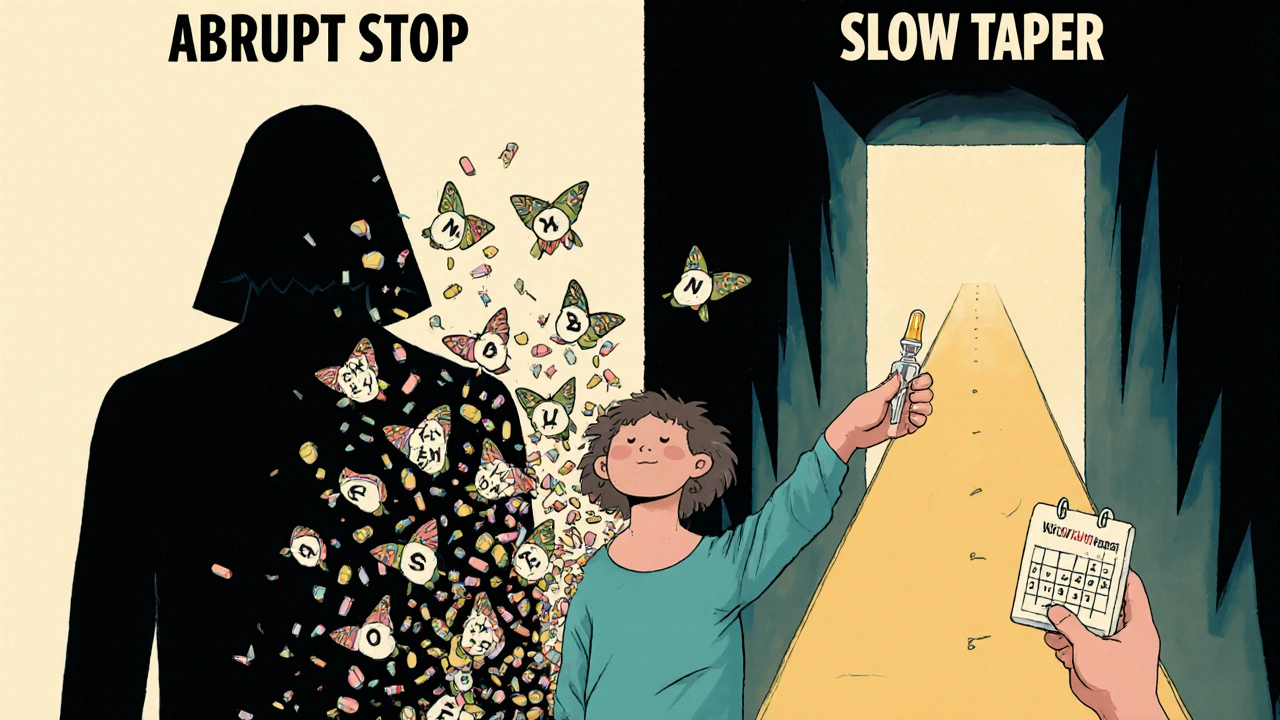
There’s only one reliable way to avoid severe withdrawal: slow tapering under medical supervision.- For most SSRIs: taper over at least 4 weeks
- For venlafaxine or paroxetine: 8 weeks or longer
- For MAOIs or TCAs: always under close doctor supervision
When to Call Your Doctor
Don’t ignore these signs:- Sudden, severe dizziness or loss of balance
- Brain zaps that feel like seizures
- Thoughts of self-harm or suicide
- Psychotic symptoms: hallucinations, delusions
- Symptoms that worsen after 2 weeks
What Doesn’t Work
- Herbal supplements: St. John’s Wort can interact dangerously with antidepressants and isn’t proven to ease withdrawal. - Alcohol or benzodiazepines: These might temporarily dull symptoms but create new risks and dependencies. - "Just push through it": Severe withdrawal can be disabling. Rest, hydration, and medical support are not signs of weakness. - Self-tapering with internet advice: Reddit threads and YouTube videos aren’t medical guidance. Dose reductions need to be personalized.What Helps During Withdrawal
While you’re tapering:- Stay hydrated. Nausea and dizziness worsen with dehydration.
- Get gentle movement-walking, yoga. Balance improves with time.
- Avoid caffeine and sugar. They can spike anxiety and disrupt sleep.
- Use a symptom tracker. Note when symptoms start, how bad they are, and what you were doing. This helps your doctor adjust your plan.
- Ask for emotional support. Withdrawal can feel isolating. Talk to someone who understands.
Final Thought: Your Experience Matters
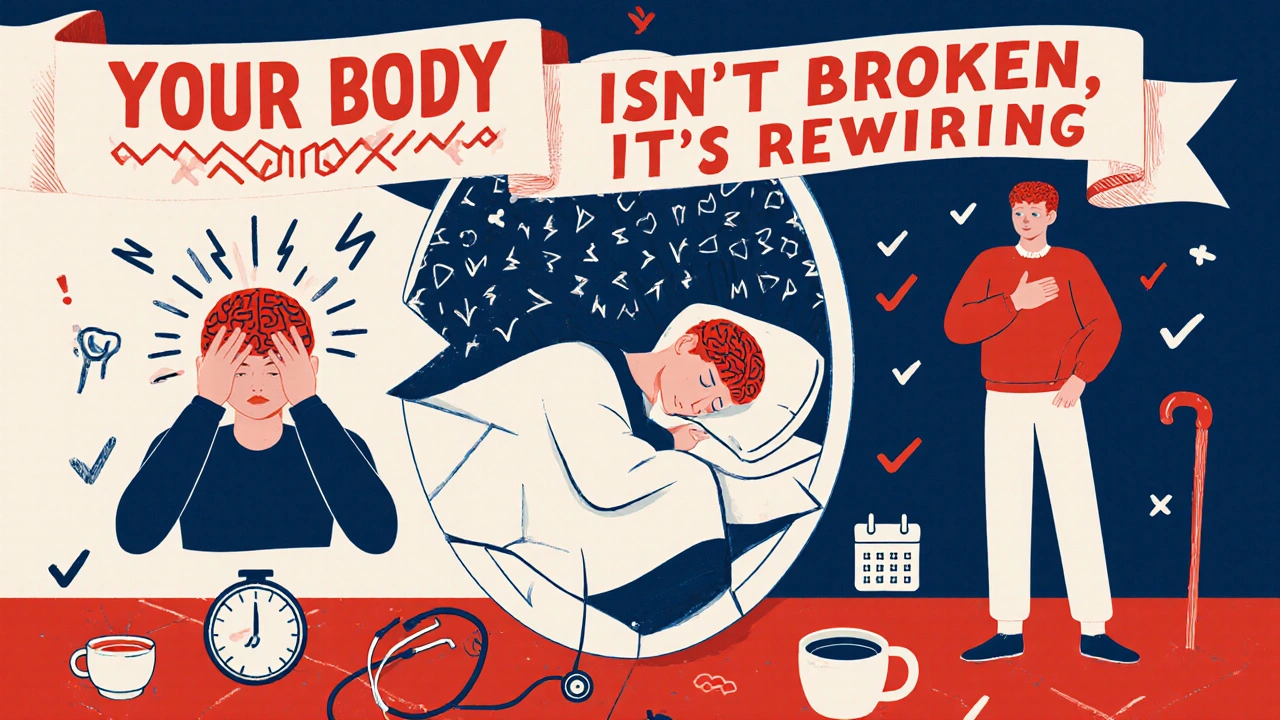
Too many people are told, "It’s all in your head," or "It’s just anxiety returning." But the science is clear: your body is reacting to a chemical shift. You’re not broken. You’re not weak. You’re experiencing a physiological response that’s been underdiagnosed for decades. If you’re thinking about stopping your antidepressant, don’t do it alone. Talk to your prescriber. Ask about tapering. Ask about alternatives. Ask for a plan. And if you’ve already stopped and are suffering-reach out. Symptoms can still be managed. Recovery is possible.Can antidepressant withdrawal cause permanent damage?
There’s no evidence that antidepressant withdrawal causes permanent brain damage. Symptoms are caused by temporary neurochemical imbalance. Most people fully recover, even those with protracted symptoms. The nervous system is highly adaptable. Recovery takes time, but it’s not permanent. Ongoing research is focused on understanding why some people take longer to heal, but no structural brain changes have been confirmed.
Why do I get brain zaps when I move my eyes?
"Brain zaps" are believed to be caused by sudden changes in serotonin signaling in the brainstem and visual pathways. When you move your eyes rapidly, it triggers a neural pathway that’s hypersensitive after antidepressant withdrawal. This is why they often happen when turning your head, looking up, or blinking quickly. They’re not seizures or strokes-they’re harmless, though deeply unsettling. They usually fade within weeks as your brain re-stabilizes.
Can I stop my antidepressant if I feel fine?
Feeling fine doesn’t mean you’re ready to stop. Antidepressants are often prescribed for 6-12 months after symptoms improve to prevent relapse. Stopping too early increases your risk of depression returning. Even if you feel great, consult your doctor before stopping. They can help you decide if you’re truly stable and create a safe tapering plan.
Is it safe to quit antidepressants during pregnancy?
Quitting antidepressants during pregnancy without medical advice carries risks. Untreated depression can affect fetal development, and abrupt withdrawal can trigger severe anxiety or mood episodes in the mother. Some antidepressants, like sertraline and fluoxetine, are considered relatively low-risk during pregnancy. The decision should be made with your OB-GYN and psychiatrist together-never on your own.
What if my doctor says withdrawal isn’t real?
If your doctor dismisses your symptoms, seek a second opinion. Antidepressant discontinuation syndrome is recognized by the American Academy of Family Physicians, the Royal College of Psychiatrists, and the National Institutes of Health. It’s listed in the DSM-5 under "Other Conditions That May Be a Focus of Clinical Attention." You have the right to be heard. Bring printed guidelines or ask for a referral to a psychopharmacologist.







Ravi boy
November 20, 2025 AT 09:10bro i stopped sertraline cold turkey last year and thought i was dying. brain zaps felt like my skull was getting electrocuted every time i blinked. took me 3 months to feel normal again. no one warned me. dont be like me
Matthew Peters
November 22, 2025 AT 04:50i used to think these symptoms were just anxiety until i started tracking them. the timing was always 24-48 hours after missing a dose. i switched to fluoxetine for tapering and it was like flipping a switch. the brain zaps didn’t vanish overnight but they went from terrifying to annoying. patience isn’t a virtue here-it’s the only treatment that works
Michael Fessler
November 23, 2025 AT 18:30as a psych nurse i’ve seen this too many times. patients come in panic-ing about "new depression" but their last dose was 72 hours ago. they’re not relapsing-they’re in withdrawal. the key is recognizing the FINISH mnemonic. flu-like + sensory + imbalance = discontinuation syndrome. never assume it’s psychological. check the half-life. if it’s venlafaxine or paroxetine? you’re looking at a 6-8 week taper minimum. and no, cutting pills in half doesn’t cut it. you need compounding pharmacies for micro-dosing
Liam Strachan
November 24, 2025 AT 14:27i’m glad this got posted. my sister thought she was going crazy after quitting citalopram. her doctor told her it was "just stress." she ended up in the ER because of the dizziness. took three specialists and a year before anyone took her seriously. this info should be mandatory reading for every gp
Ron and Gill Day
November 25, 2025 AT 23:34this is why i stopped reading medical content on the internet. everyone’s an expert. you think you know about neurochemistry? i’ve got a phd in pharmacology and i still don’t trust half of what’s written here. who funded this? big pharma wants you scared so you keep taking pills. the real issue is that we overprescribe these drugs like candy. and now you’re all terrified of coming off them? pathetic
Matthew Karrs
November 26, 2025 AT 11:12i’ve been watching this for 8 years. the FDA doesn’t require manufacturers to test withdrawal effects. the 40% statistic? it’s from patient surveys. the drug companies buried the data. they know paroxetine causes brutal withdrawal but they market it as "safe" because it’s profitable. and don’t get me started on the generic switch scams. i switched from brand zoloft to a $5 generic and woke up with brain zaps. the FDA says they’re bioequivalent. i say they’re lying. this isn’t science. it’s corporate cover-up
daniel lopez
November 27, 2025 AT 22:21this is why america is broken. you people are so addicted to chemical crutches you can’t even handle being human. depression isn’t a brain chemical imbalance-it’s a failure of will. if you just exercised more, got sunlight, and stopped whining, you wouldn’t need this stuff. and now you want a 6-month taper because your brain can’t handle reality? pathetic. just quit. grow up. stop being a victim
Gerald Cheruiyot
November 28, 2025 AT 23:44the nervous system is a living thing. it adapts. it remembers. when you remove the drug, it doesn’t just flip back on. it has to relearn how to regulate itself without the crutch. that’s not weakness. that’s biology. the fact that we treat this like a personal failure instead of a physiological event is what’s broken. recovery isn’t about willpower. it’s about time, patience, and respect for the body’s intelligence