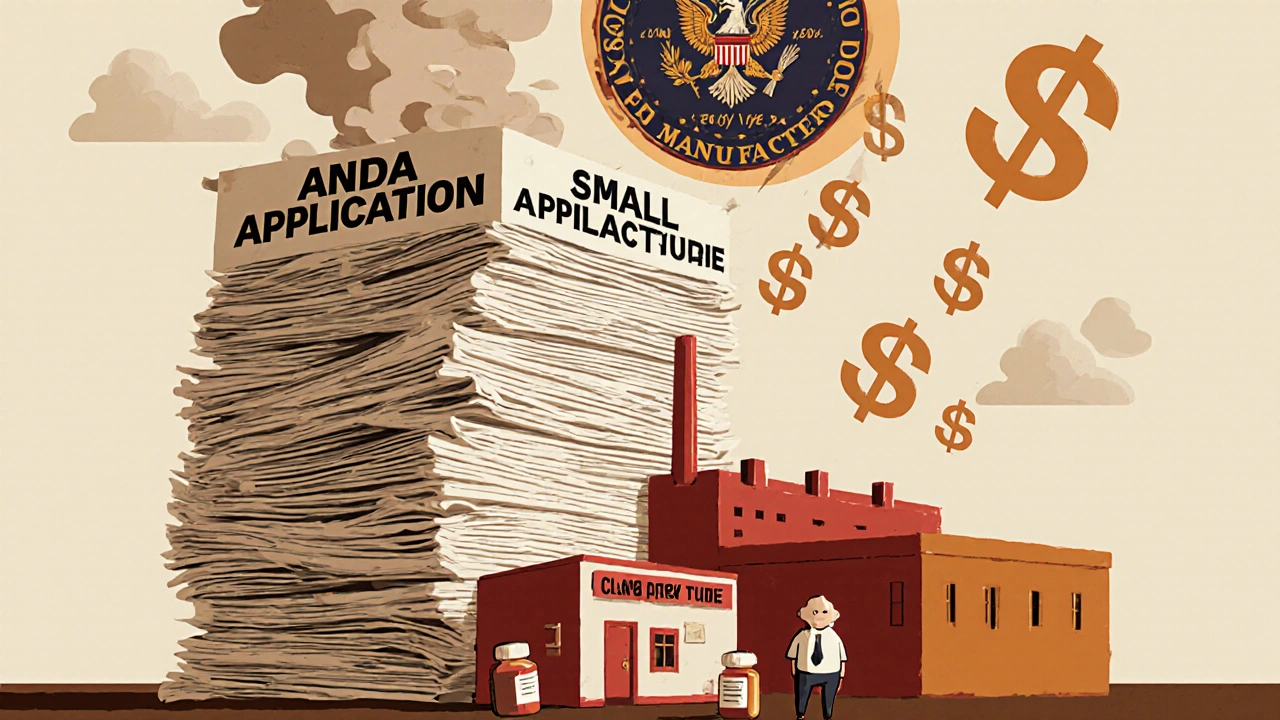
It costs over $375,000 just to apply for FDA approval of a single generic drug. For many small manufacturers, that’s more than their entire annual budget. And if the FDA sends back the application - which happens nearly 60% of the time for complex generics - they’re looking at another $2 million and a year-long delay. This isn’t just bureaucracy. It’s a hidden tax on every prescription you fill.
What You’re Really Paying For
You might think generic drugs are cheap because they’re simple copies. They’re not. A generic version of a brand-name drug isn’t just a repackage. It has to match the original in every way: how it dissolves, how it’s absorbed, even how it looks. The FDA requires proof - and that proof is expensive.
The main cost comes from the Abbreviated New Drug Application (ANDA). Under GDUFA III, which runs through 2027, each application carries a $136,485 product fee, plus $238,055 in facility fees if you manufacture the drug. Add in legal, testing, and documentation costs, and you’re easily at $375,000 before you even submit. Compare that to a brand-name drug, which costs over $3.6 million to get approved. The math seems fair - until you realize generics make up 90% of all prescriptions but only 12% of total drug spending.
That’s the trade-off: the system is designed to keep prices low. But the cost of getting there is crushing smaller companies. In 2024, the FDA approved over 1,000 generic drugs - a record. But nearly 300 applications sat in limbo because of patent fights or manufacturing issues. That means fewer generics on shelves, and higher prices for patients.
The Hidden Cost: Complex Generics
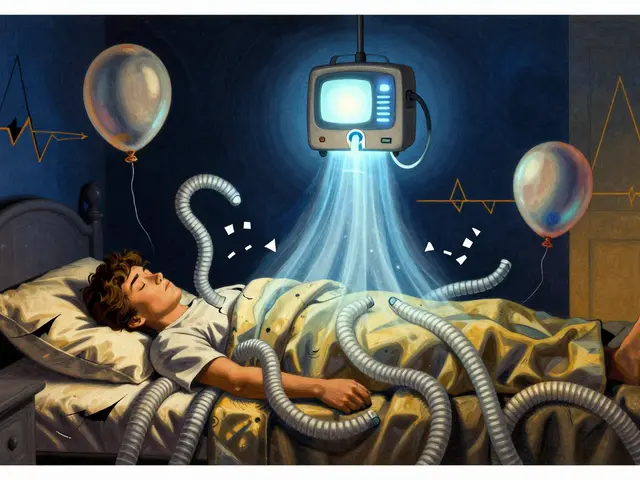
Not all generics are created equal. A simple tablet you swallow? Easy. A nasal spray, injectable, or patch that needs to deliver the drug in a very specific way? That’s a complex generic. These make up about 15% of the pipeline but cause 70% of the delays.
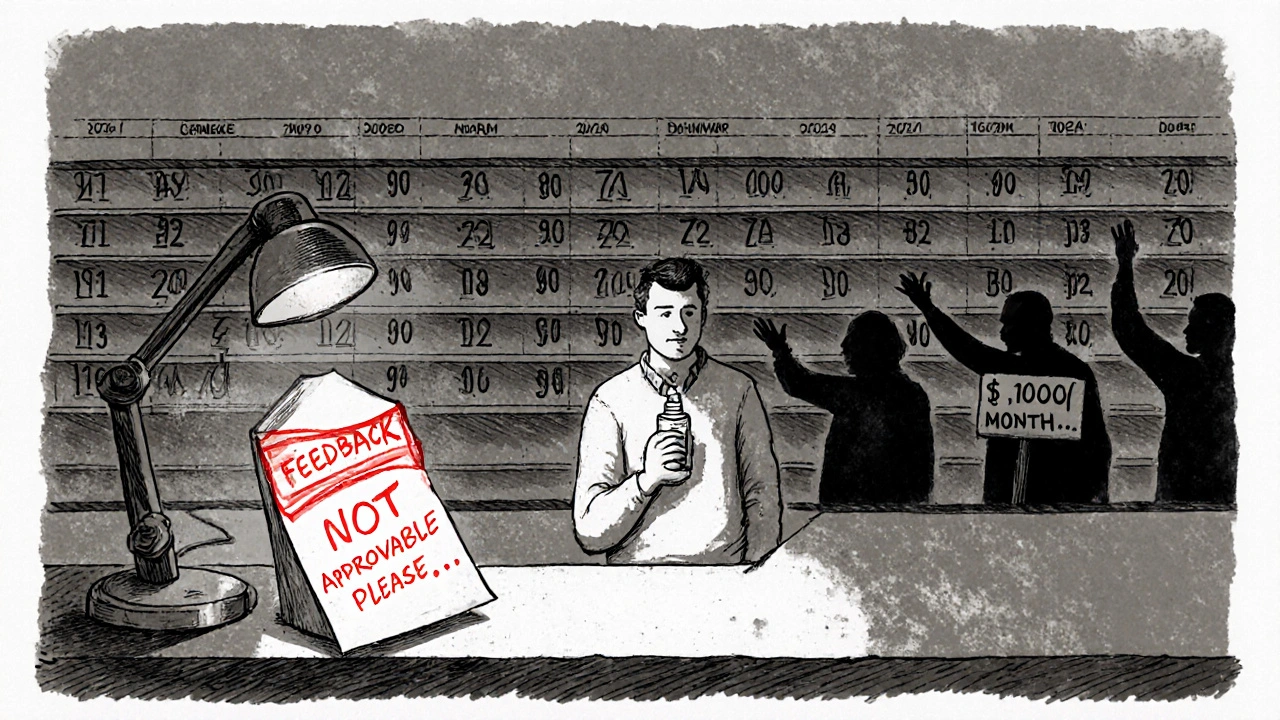
Here’s the problem: since 2015, the FDA stopped giving specific feedback on formulation issues. If your generic nasal spray doesn’t match the brand’s particle size or viscosity, they won’t tell you why. They just say ‘not approvable’ and send it back. Companies have to guess. And guess wrong. And guess again.
One mid-sized manufacturer told RAPS in 2024 they spent $8.7 million on three failed reformulations of a single nasal spray. Each attempt took 18 months. That’s $2.9 million per try - just to get the chemistry right. Meanwhile, the brand-name version kept selling at full price. Patients paid 300% more for years. The delay for generic testosterone replacement therapy? Nearly five years. That’s thousands in out-of-pocket costs for people who just need affordable medication.
Review Times Are Slowing Down
GDUFA III promised 10-month reviews for standard applications. In 2023, the actual average was 11.2 months. For complex generics? It’s closer to 18 months. Why? Because the applications are bigger - now averaging 150,000 to 200,000 pages of data. That’s triple the size of what they were in 2013. Reviewers are overwhelmed.
And when they do send back a Complete Response Letter (CRL), it’s often vague. ‘Insufficient data.’ ‘Not equivalent.’ No specifics. That forces manufacturers to rebuild entire batches, run new clinical tests, and resubmit. Each CRL adds $2-5 million and 8-12 months. For a company with limited cash flow, that’s a death sentence.
Companies that survive do one thing: they talk to the FDA early. According to the Association for Accessible Medicines, 78% of successful applicants held Type II meetings before submitting. These are pre-submission chats where you can ask, ‘Will this formulation work?’ - and get an answer. Skip that step, and you’re gambling $300,000 on a guess.
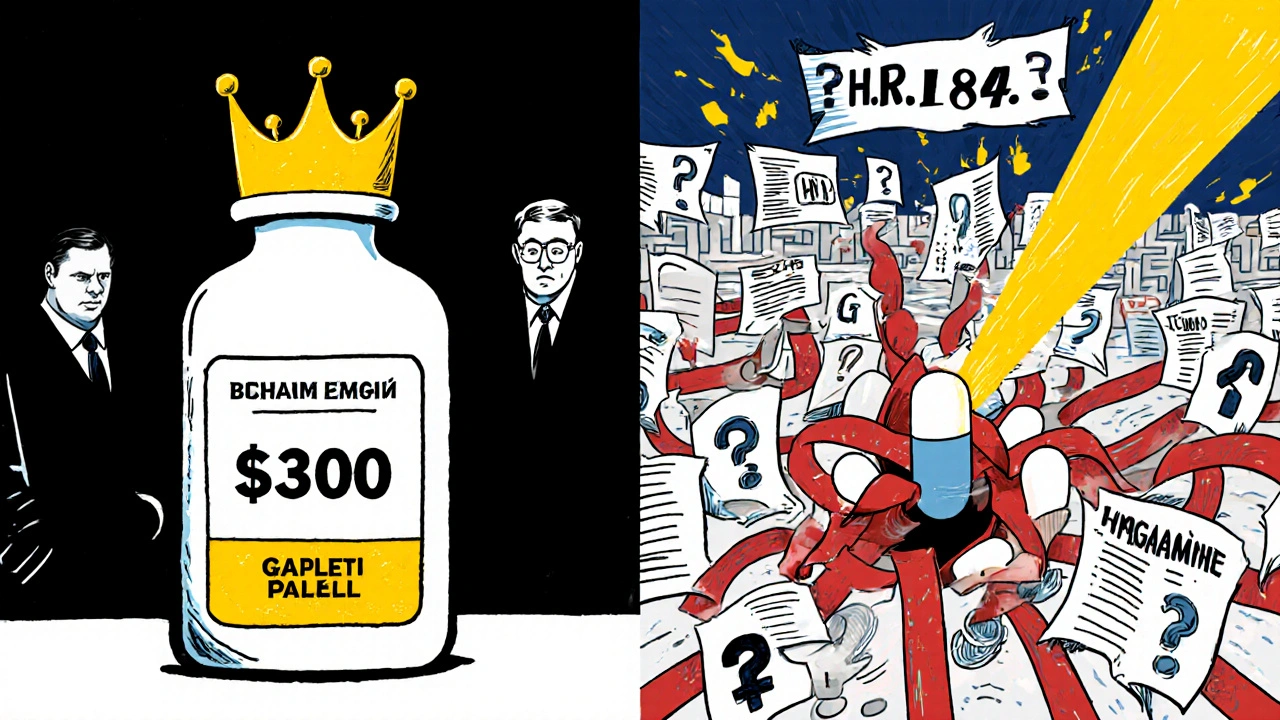
Who’s Winning? Who’s Losing?
The big players - Teva, Sandoz, Mylan - can absorb these costs. They have legal teams, in-house chemists, and cash reserves. But smaller companies? They’re vanishing. Since 2018, over 120 generic manufacturers have closed or been bought out, according to IQVIA. That means less competition. Less competition means fewer price drops.
Meanwhile, brand-name companies benefit. Even after their patents expire, 83% of drugs still have no generic competitor after five years. Why? Because the FDA process is too slow, too expensive, and too unpredictable. So the original maker keeps charging high prices - and patients pay the price.
But here’s the real kicker: generics saved the U.S. healthcare system $467 billion in 2024. That’s $1,152 per Medicare beneficiary. That’s billions in savings for insurers, employers, and taxpayers. And yet, the system is designed in a way that makes it harder to produce those savings.
What’s Changing? The Push for Reform
In September 2025, Congress introduced H.R. 1843 - the ‘Increasing Transparency in Generic Drug Applications Act.’ It’s rare to see bipartisan support on drug policy, but this bill has 72 co-sponsors. Why? Because it’s simple: force the FDA to give clear, written feedback on formulation problems.
The Congressional Budget Office estimates this could cut approval times for complex generics by 18-24 months. That means 12-15 more complex generics hit the market each year. The savings? $1.8 to $2.3 billion annually. Over five years, that’s $18-23 billion.
The FDA isn’t opposed to change - but they’re scared. In July 2025, their Office of Generic Drugs warned that giving more feedback without more staff could lead to mistakes. They’re caught between speed and safety. But patients aren’t waiting. On Reddit’s r/pharmacy, a September 2025 thread titled ‘Generic approval delays cost me $1,200/month’ had 147 comments. People are paying thousands for drugs that should cost $10.
What This Means for You
If you take a generic drug, you’re already saving money. But if that drug is a nasal spray, inhaler, or injectable, you might be waiting years for a cheaper version. And if you’re paying out of pocket, those delays hit harder.
Here’s what you can do:
- Ask your pharmacist: ‘Is there a generic version of this drug that’s been approved?’ If not, ask why.
- Check the FDA’s Orange Book online. It lists approved generics and patent status. If a drug has no generic after five years, it’s likely stuck in the system.
- Support policy changes. H.R. 1843 could be the biggest boost to affordable drugs in a decade.
The system isn’t broken because it’s greedy. It’s broken because it’s overloaded. The FDA wants to approve generics fast. But they’re underfunded, understaffed, and bound by rules that were meant to protect safety - but now protect profits.
Every delay in approval is a tax on the sick. Every vague rejection letter is a hidden cost you pay at the pharmacy counter. And every time a small manufacturer gives up, you lose a chance for a cheaper drug tomorrow.
How much does it cost to get a generic drug approved by the FDA?
For a standard generic drug, the total cost is around $375,000. This includes a $136,485 product fee, a $238,055 facility fee, and additional costs for testing, documentation, and legal work. For complex generics - like nasal sprays or injectables - costs can jump to $1 million or more due to multiple reformulation attempts and longer review times.
Why are generic drug approvals taking so long?
The FDA’s review process is backlogged. Applications have grown from 50,000 pages to over 200,000 pages since 2013. For complex generics, the FDA stopped giving specific feedback in 2015, forcing manufacturers to guess what’s wrong. This leads to multiple rejections and delays of 18-24 months. Average review times are now 11.2 months for standard drugs and up to 18 months for complex ones.
What’s the difference between a brand-name and generic drug approval cost?
A brand-name drug (NDA) costs about $3.685 million to get approved under PDUFA. A generic drug (ANDA) costs roughly $375,000 - about 10% of the price. But while the upfront cost is lower, complex generics can end up costing more due to repeated failures and reformulations, making the path to market longer and riskier.
Why do some generic drugs never come to market?
Many generics never launch because the approval process is too expensive or too uncertain. Small manufacturers can’t afford multiple failed attempts. Patent lawsuits also delay entry - 287 applications were pending due to patent issues in 2024. Even after approval, some companies decide the market isn’t big enough to justify the cost of manufacturing.
How do FDA approval delays affect patients?
Delays mean patients pay higher prices for longer. For example, generic testosterone replacement therapy was delayed for 4.7 years - during which patients paid 300% more. On average, patients save $1,152 per year on Medicare Part D thanks to generics. But when those generics are blocked, those savings disappear. Reddit threads and patient advocacy groups report out-of-pocket costs of $1,000-$2,000 per month for drugs that should cost under $50.
What’s Next?
The FDA is now preparing for GDUFA IV, the next five-year funding cycle starting in 2028. Industry groups want fee increases of 3-5% per year to hire more reviewers. The FDA says they need $725-750 million annually to meet goals. Congress is watching - and H.R. 1843 could change everything.
If that bill passes, the next time you walk into a pharmacy and see a new generic version of your expensive medication, you’ll know why: it wasn’t luck. It was policy.




Hannah Blower
November 17, 2025 AT 21:03The FDA isn't broken-it's *designed* this way. You think this is about safety? Nah. It's about rent-seeking. Big pharma lobbied for these fees so small players couldn't compete. The ‘complex generic’ loophole? That’s not a regulatory gap-it’s a corporate moat. And now we’re all paying the toll, one $1,200 monthly prescription at a time. The system doesn’t fail-it *succeeds* at protecting profits under the guise of safety. Wake up.
Gregory Gonzalez
November 18, 2025 AT 19:21Oh wow. $375k to make a pill? How dare they charge so little. I mean, I’m sure the FDA reviewers are just sitting around sipping lattes while your ‘life-saving’ nasal spray gets rejected for the 4th time. How quaint. Maybe if you spent less time crying about costs and more time learning chemistry, you wouldn’t need a government handout to make a drug that works.
Ronald Stenger
November 20, 2025 AT 01:59Let’s be real-this is a national security issue. China and India are flooding the market with cheap generics because our FDA is too slow. Every delay means more Americans die waiting for insulin or testosterone. We’re outsourcing our health to foreign labs while our own regulators play bureaucratic whack-a-mole. This isn’t about cost-it’s about sovereignty. If we can’t make our own pills, we’re not a country. We’re a pharmacy.
Samkelo Bodwana
November 21, 2025 AT 09:55Look, I come from a place where people wait months for basic antibiotics, and here you're debating whether a nasal spray costs $2 million to approve. I don't say this to diminish your struggle-I say it to remind you that privilege is measured in how much bureaucracy you can afford to navigate. The FDA’s delays are tragic, yes. But so is the fact that 70% of the world can't even get a basic generic. Maybe the real reform isn't just faster reviews-it's global equity. We need to stop treating medicine like a luxury product with a waiting list.
Emily Entwistle
November 22, 2025 AT 15:44Y’all are right. This is so messed up 😭 I just got my prescription for my asthma inhaler and it’s $180… and there’s a generic that’s been approved since 2023 but STILL not on shelves?? 🤦♀️ I’m so mad I could scream. Let’s sign that bill!! 💪 #GenericJustice 🙏
Duncan Prowel
November 22, 2025 AT 17:26It is worth noting that the GDUFA III framework, while ostensibly designed to expedite approvals, has paradoxically increased the administrative burden on applicants due to the expansion of data requirements without a proportional increase in reviewer capacity. The phenomenon of the Complete Response Letter-often lacking granular detail-suggests a systemic misalignment between regulatory intent and operational capability. One might posit that the current model is not merely inefficient, but structurally unsustainable absent significant investment in human capital and transparency protocols.
Bruce Bain
November 23, 2025 AT 04:59So let me get this straight. You pay $375k just to ask if your pill works? And if they say no, you pay $2 million to try again? That’s like buying a car, then paying $20k to find out if the tires fit. Why not just give people the pill and see if it works? We don’t need a PhD to make a generic. We need common sense. This isn’t rocket science. It’s medicine.
Jonathan Gabriel
November 23, 2025 AT 19:10okay so i read this whole thing and my brain is like… why does the FDA even exist if they don’t give feedback? like if you’re gonna reject me, tell me why. did my tablet have the wrong shade of blue? is my viscosity not *aesthetic* enough? 🤡 the fact that companies spend millions guessing is criminal. and the 150k-page applications? that’s not science, that’s a parody of bureaucracy. someone at the FDA is getting paid to read 200k pages of PDFs and say ‘insufficient data’? i’d rather be a potato.
Don Angel
November 25, 2025 AT 13:47I’ve been in this game for 18 years. I’ve seen startups go under because of one vague CRL. I’ve sat in rooms with FDA reviewers who said, ‘We don’t know what’s wrong, but it’s not right.’ That’s not regulation. That’s intimidation. And now we’re supposed to cheer because 1,000 generics got approved? Meanwhile, 300 are rotting in limbo. This isn’t progress. It’s a slow-motion collapse. And the worst part? No one’s listening until someone dies.
benedict nwokedi
November 26, 2025 AT 10:43Wait… wait… wait. Let me get this straight. The FDA is controlled by Big Pharma? And they’re using ‘safety’ as a cover to block generics? And now Congress is pushing a bill to force them to give feedback? That’s… that’s not reform. That’s a Trojan horse. The FDA doesn’t want transparency-they want control. And if you think this is about patients, you’re naive. This is a power play. They’re scared of losing the leash. And when they lose it? The next thing you know, you’ll be getting your insulin from a blockchain app. Don’t trust the system. It’s rigged.
deepak kumar
November 27, 2025 AT 14:09In India, we make generics for pennies-but we still follow the science. The problem isn’t the cost-it’s the lack of standardization in feedback. If the FDA gave clear, technical reasons for rejection-like ‘particle size exceeds 5 microns’-companies could fix it in weeks, not years. I’ve worked on a generic inhaler that took 14 months to fix because we had to reverse-engineer the brand’s spray pattern. With clear feedback? Three months. This isn’t about money. It’s about communication. And the FDA needs to stop acting like a black box.
Dave Pritchard
November 28, 2025 AT 22:42If you’re reading this and you’re stressed about your meds, I see you. I’ve been there. My mom waited two years for a generic thyroid med. She paid $300/month until one finally came out. You’re not alone. The system’s broken, but change is coming. H.R. 1843 isn’t perfect-but it’s a start. Talk to your pharmacist. Share this post. Tell your rep. We don’t need to fix everything today. We just need to start. And you? You’re already doing your part by caring. That matters more than you know.