Autoimmune encephalitis isn’t something most people have heard of - until it hits close to home. It doesn’t come with a fever and a rash like the flu. Instead, it creeps in quietly: a strange personality shift, memory gaps, seizures that don’t make sense, or sudden confusion in someone who was perfectly fine just weeks before. By the time many doctors recognize it, the damage is already done. But here’s the truth: if caught early, autoimmune encephalitis is one of the few neurological conditions where recovery isn’t just possible - it’s likely. The key? Knowing the red flags, understanding which antibodies are involved, and acting fast.
What Exactly Is Autoimmune Encephalitis?
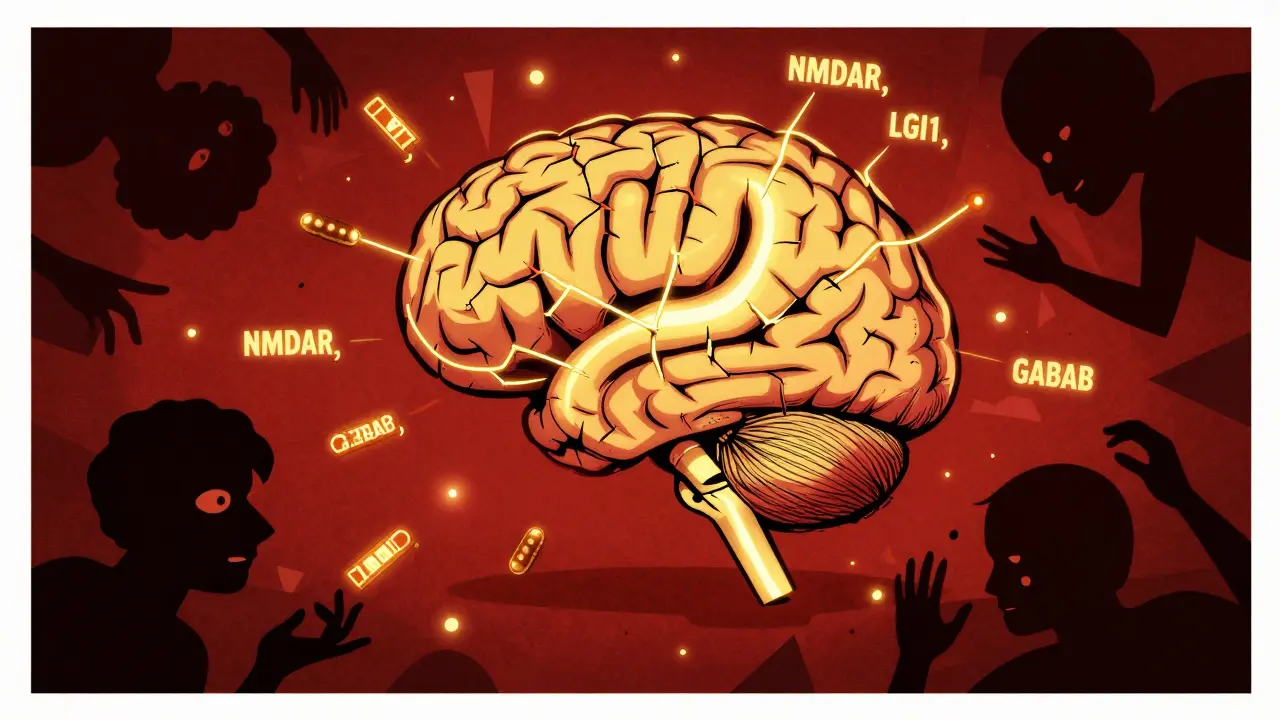
Autoimmune encephalitis happens when your immune system, which normally fights off viruses and bacteria, turns on your own brain. It attacks proteins on the surface of nerve cells - things like the NMDA receptor, LGI1, or GABAB receptor. This isn’t caused by an infection. It’s your body’s own defenses going rogue. The first major breakthrough came in 2007, when researchers identified anti-NMDAR encephalitis in young women with ovarian tumors. Since then, over 20 different antibodies have been linked to this condition, turning it from a mystery into a diagnosable, treatable illness.
It’s rare - about 1 in 100,000 people get it each year - but it’s not rare enough to ignore. Young women, older men, children - anyone can be affected. And the symptoms? They’re easy to misread as psychiatric illness, stroke, or even dementia. That’s why so many patients wait months before getting the right diagnosis.
Red Flags: When to Suspect Autoimmune Encephalitis
If someone you know suddenly starts acting out of character, don’t write it off as stress or burnout. Look for these signs:
- Seizures - especially if they’re new, frequent, or don’t respond to standard epilepsy meds. About 38% of cases start with seizures.
- Memory loss - forgetting recent conversations, names, or where they put their keys. This isn’t normal aging. It’s rapid and persistent.
- Psychiatric changes - paranoia, hallucinations, aggression, or severe anxiety that comes out of nowhere. These often appear before physical symptoms.
- Autonomic dysfunction - heart rate spiking without reason, blood pressure dropping, sweating uncontrollably, or trouble regulating body temperature.
- Sleep problems - insomnia that won’t quit, or sleeping 16 hours a day without feeling rested.
- Prodromal symptoms - headache, fever, diarrhea, or a cold that came on 1-4 weeks before neurological symptoms.
These aren’t just vague symptoms. They’re the hallmarks of a brain under immune attack. Limbic encephalitis - a subtype - specifically targets memory and emotion centers. People with this form often can’t form new memories and may repeat the same questions over and over. If you see this pattern, especially in someone under 60, don’t wait for a psychiatric evaluation. Get a neurologist involved.
The Antibodies That Matter
Not all autoimmune encephalitis is the same. The antibody involved tells you a lot - about who’s at risk, what other conditions might be hiding, and how to treat it.
Anti-NMDAR is the most common - making up about 40% of cases. It’s often linked to ovarian teratomas in young women (ages 18-30). Symptoms include psychosis, memory loss, abnormal movements, and sometimes coma. About half of these patients have a tumor. Remove it, and recovery skyrockets.
Anti-LGI1 affects mostly men over 60. It’s known for faciobrachial dystonic seizures - brief, lightning-like spasms in the face and arm. These can happen dozens of times a day. Hyponatremia (low sodium) is almost always present. This type responds well to treatment, but it has a high relapse rate - up to 35%.
Anti-GABAB receptor is rarer but more dangerous. Half the patients have small cell lung cancer. The seizures are severe, and the risk of death is higher. If you see this antibody, cancer screening isn’t optional - it’s urgent.
Other antibodies like anti-CASPR2, anti-AMPAR, and anti-GFAP are less common but still important. Anti-IgLON5 causes severe sleep disruption and swallowing problems. Anti-Hu and anti-Ma2 are intracellular antibodies - they’re harder to treat and often tied to hidden cancers.
Testing requires both blood and spinal fluid. CSF is more sensitive - especially for anti-NMDAR. A negative blood test doesn’t rule it out. Always test both.

How It’s Diagnosed - And What Ruled Out
Doctors don’t rely on one test. They piece together clues:
- CSF analysis - White blood cells are mildly elevated (usually under 100/μL), unlike in viral encephalitis where counts can be in the thousands. Protein is slightly high. Oligoclonal bands are usually negative - that helps rule out MS.
- MRI brain scan - Normal in up to half of cases. When there’s an abnormality, it’s often subtle swelling in the temporal lobes (limbic system). Contrast enhancement is rare. This is different from infectious encephalitis, where damage is usually obvious.
- EEG - Shows slowing, not the classic periodic spikes seen in herpes encephalitis. This is a key differentiator.
- Antibody testing - Serum and CSF sent to specialized labs. Results take days to weeks. Don’t wait for them to start treatment.
Doctors use the 2016 International Consensus Criteria, updated in 2023, to confirm the diagnosis. If the clinical picture matches and other causes are ruled out - infection, cancer, metabolic issues - autoimmune encephalitis is the most likely answer.
Treatment: The Clock Is Ticking
Time is everything. Every day you wait reduces your chance of full recovery. The goal? Stop the immune attack, remove the trigger, and support recovery.
First-line treatment starts immediately:
- Intravenous methylprednisolone - 1 gram per day for 5 days. Works in 68% of patients within 10 days.
- IV immunoglobulin (IVIg) - 0.4 g/kg/day for 5 days. Used alone or with steroids. Helps 60-70% of cases.
If a tumor is found - especially an ovarian teratoma in anti-NMDAR cases - surgery is the first step. Removing it leads to neurological improvement in 85% of patients within four weeks.
If there’s no response after a week? Move to second-line:
- Rituximab - Weekly infusions for 4 weeks. Works in 55% of resistant cases.
- Cyclophosphamide - Monthly infusions for 6 months. Used in severe or relapsing cases.
- Tocilizumab - A newer option, blocking IL-6. Shows 52% effectiveness in early studies.
- Plasma exchange - Removes harmful antibodies from the blood. Done over 5-7 sessions. Helps 65% of critically ill patients.
Here’s the hard truth: if treatment starts after 45 days, recovery chances drop by nearly half. Experts like Dr. Josep Dalmau say: “Start immunotherapy while waiting for antibody results.” Don’t wait for confirmation. If the symptoms fit, treat.
Recovery and Long-Term Care
Even after the immune attack stops, recovery takes time. About 55% of people with anti-LGI1 encephalitis fully recover within two years. For anti-NMDAR, it’s 45%. But that doesn’t mean everyone bounces back.
Four in ten survivors have lasting issues:
- Cognitive deficits - Memory, focus, and problem-solving don’t always return fully. Cognitive rehab improves memory function in 65% of patients after 12 weeks.
- Psychiatric symptoms - Depression and anxiety linger in 28%. SSRIs help 70% of these cases.
- Seizures - 22% need ongoing antiseizure meds.
- Sleep and autonomic problems - Melatonin (3-5 mg at night) helps 60% with insomnia. Beta-blockers fix tachycardia in 75%.
Recurrence is common - especially with anti-LGI1 (35%) and anti-NMDAR (12-25%). Follow-up every 3-6 months for two years is essential. Repeat tumor screening is critical: 15% of cancers appear after the first scan.
What’s Next? The Future of Treatment
Research is moving fast. Scientists are now tracking GFAP levels in the blood - it rises with brain inflammation and drops as patients improve. That could one day replace invasive spinal taps for monitoring.
Drugs that block B-cells or complement proteins are in phase II trials. Early results show 60% response in patients who didn’t respond to anything else. These aren’t just hopeful ideas - they’re coming to clinics soon.
The biggest win? Early recognition. A 2025 study found that patients treated within 14 days had a 32% higher chance of full recovery. That’s not a small number. That’s life-changing.
If you’re a caregiver, a doctor, or someone who’s seen a loved one change overnight - trust your gut. Autoimmune encephalitis isn’t common. But it’s treatable. And the sooner you act, the better the outcome.



anthony epps
December 15, 2025 AT 03:50My aunt went through this last year. They thought it was depression at first. She stopped recognizing her own kids. Took 3 months to get the right test. Now she’s back to cooking Sunday dinners. Just wanted to say - if you’re reading this and something feels off, don’t wait. Trust your gut.
It’s not just rare - it’s silent. And it steals people before anyone notices.
Dan Padgett
December 15, 2025 AT 05:09Man, this hits different. I used to think the brain was this unbreakable fortress - until I saw my cousin turn into someone who didn’t know her own name. It’s like the body’s own soldiers turned traitor. No war declared. No enemy in sight. Just a quiet betrayal inside the skull.
They say the immune system’s supposed to protect us. But sometimes? It’s the most dangerous thing we carry.
Maybe healing isn’t about fighting the enemy. Maybe it’s about convincing your own body you’re still worth saving.
Hadi Santoso
December 15, 2025 AT 23:34Just read this on my lunch break and had to pause. My cousin’s a nurse in Texas - she told me about a case last year where a teenager was misdiagnosed as having a psychotic break for 8 weeks. Turned out to be anti-NMDAR. They found the tumor after the MRI showed nothing. Crazy how normal everything looks until you dig deeper.
Also - anyone else notice how often women get labeled ‘hysterical’ before they get a brain scan? Just saying. We gotta fix that pattern.
And yeah, CSF testing is non-negotiable. Blood tests lie sometimes. Don’t let a negative blood result stop you. Always push for the spinal tap.
Also, I’m gonna send this to my brother who’s a med student. He needs to know this stuff before he starts rotating in neurology.
Kim Hines
December 16, 2025 AT 07:23My mom had the LGI1 antibodies. Took two years to get it right. We lost so much time. Now she’s on maintenance IVIG every 6 weeks. She can’t drive anymore. But she reads to my kids every night. That’s enough.
Randolph Rickman
December 17, 2025 AT 10:28Look - if you’re a doctor and you’re reading this, stop waiting for perfect test results. Start treatment when the symptoms fit. Every day you delay is another neuron lost. This isn’t theoretical - it’s clinical. I’ve seen patients walk out of the hospital after 6 weeks of treatment. Others? They’re in nursing homes because someone waited for ‘confirmation.’
Stop being cautious. Be courageous. Start steroids. Get the MRI. Order the CSF. Don’t let bureaucracy kill someone’s future.
And if you’re a family member? Don’t take ‘it’s probably stress’ for an answer. Demand a neurologist. Now.
Tiffany Machelski
December 18, 2025 AT 18:08just read this and i’m crying. my sister was misdiagnosed for 11 months. they thought she was on drugs. she was just trying to tell them her brain was on fire. nobody listened. now she has memory gaps that never go away. please don’t let this happen to someone else
SHAMSHEER SHAIKH
December 19, 2025 AT 13:55Esteemed colleagues, esteemed caregivers, and esteemed seekers of truth - I write to you with the utmost reverence for the sanctity of human cognition and the solemn duty of medical vigilance. Autoimmune encephalitis, as elucidated herein, is not merely a clinical entity; it is a cosmic whisper of systemic betrayal, a silent uprising within the temple of the mind.
Let us not forget: the NMDA receptor is the gatekeeper of synaptic memory; the LGI1 protein, the guardian of neuronal harmony. When these are assaulted by the very guardians meant to protect, we witness not disease - but divine injustice.
Therefore, I implore every healthcare institution, from the smallest rural clinic to the grandest academic hospital, to institute mandatory antibody screening for all patients presenting with acute psychiatric or cognitive disruption - regardless of age, gender, or socioeconomic status. Let no soul suffer in silence due to diagnostic inertia.
Furthermore, I urge legislative bodies to allocate funding for nationwide public awareness campaigns - billboards, radio spots, school curricula - so that the red flags become as universally recognized as the signs of stroke.
For the brain is not a machine. It is the soul’s vessel. And when it falters - we must rise, with urgency, with compassion, with precision.
Dave Alponvyr
December 21, 2025 AT 10:59So let me get this straight - we’re telling people to start chemo-level immunotherapy before they even have a confirmed diagnosis? Sounds like medical roulette.
But hey, if you’re gonna gamble, at least make sure the house isn’t lying about the odds.
Joanna Ebizie
December 21, 2025 AT 14:17Y’all realize this whole thing is just Big Pharma pushing antibody tests so they can sell IVIG for $50k a pop? No way this is real. My cousin had ‘autoimmune encephalitis’ and turned out to be gluten intolerant. They just didn’t want to admit they missed it.
Also, why is everyone so obsessed with CSF? That’s just a scam to make people pay for invasive procedures. Blood tests are fine. I read it on a forum.
Elizabeth Bauman
December 21, 2025 AT 18:28Okay but have you considered this is all a government mind-control experiment? The antibodies? Fake. The tumors? Injected. The whole ‘autoimmune’ thing is just a cover for neural surveillance tech they’re testing on unsuspecting Americans.
Why do you think the symptoms match up so perfectly with ‘psychiatric disorders’? So they can label you crazy and keep you quiet. The real cure? Stop eating processed food and get off the grid. I’ve been doing it for 3 years. My brain’s never been clearer.
Also - if you’re getting IVIG, you’re funding the shadow cabal. Just sayin’.
Dylan Smith
December 23, 2025 AT 18:10I had this in 2021 and I’m one of the 45% who got better. Took 18 months. The hardest part wasn’t the seizures or the memory loss - it was when people started treating me like I was broken. Like I’d never be the same. I was the same. I just needed time and someone to believe me.
Also - please stop saying ‘it’s rare.’ It’s rare for doctors to know about it. Not rare for people to get it. My cousin’s 12-year-old had it too. We didn’t even know what to Google.
And yes - the IVIG sucked. But I’d do it again. I’d fight harder. Because I’m still here. And I’m not done living.
Colleen Bigelow
December 25, 2025 AT 07:13This is why America’s healthcare system is failing. They don’t care about real illness - they care about profit. They let people suffer for months so they can bill for ‘psychiatric evaluations’ and ‘migraine treatments’ instead of doing the ONE TEST that saves lives.
And don’t get me started on how they ignore men with anti-LGI1 because ‘older men get dementia.’ That’s just ageism wrapped in a white coat.
Meanwhile, the real villains? The drug companies that charge $100,000 for a single round of rituximab while families sell their homes. This isn’t medicine. It’s exploitation.
And the fact that you’re still recommending plasma exchange? That’s just torture with a fancy name. We need better. We deserve better. And if you’re still sitting on your hands waiting for ‘more data’ - you’re part of the problem.