QT Prolongation Risk Assessment Tool
Medication Information
Personal Risk Factors
Results
Key Risk Factors
When you're managing a serious mental health condition like schizophrenia, the last thing you want to worry about is your heart. But for many people taking antipsychotic medications, that’s exactly what doctors are asking them to monitor: the QT interval on an ECG. It’s not just a technical detail-it’s a life-or-death measure. QT prolongation can trigger a dangerous heart rhythm called torsade de pointes, which can lead to sudden cardiac death. And the risk doesn’t come from one drug alone-it often comes from the mix.
What Is QT Prolongation, and Why Does It Matter?
The QT interval on an electrocardiogram (ECG) measures how long it takes your heart’s ventricles to recharge between beats. When this interval gets too long-called QT prolongation-it means your heart muscle is taking longer than normal to reset electrically. That delay can cause chaotic, irregular heartbeats. The most dangerous of these is torsade de pointes, a type of ventricular tachycardia that can collapse into cardiac arrest if not treated fast. Doctors correct the QT interval for heart rate, calling it QTc. A QTc over 500 milliseconds is considered clinically dangerous. An increase of more than 60 ms from your baseline also raises red flags. Even small changes matter: a 30 ms prolongation can double your risk of sudden death in some cases.Which Antipsychotics Carry the Highest Risk?
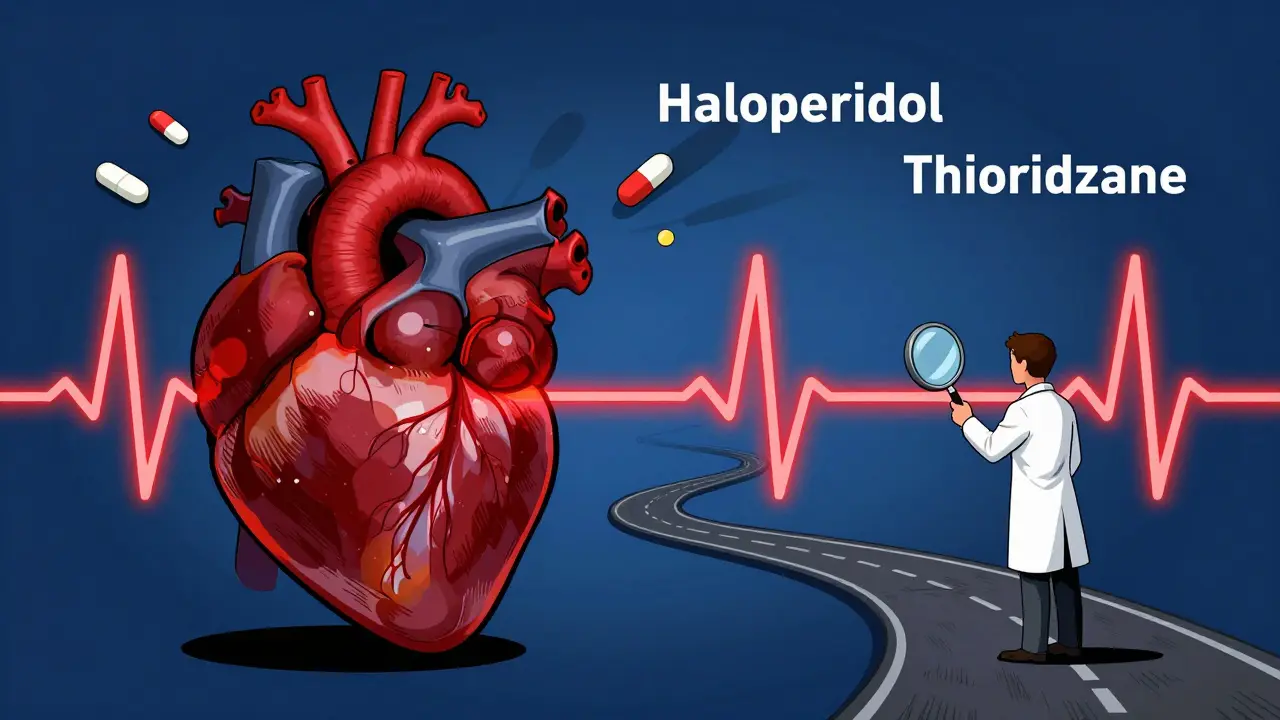
Not all antipsychotics are created equal when it comes to heart safety. The risk varies dramatically-from nearly harmless to seriously dangerous.- Thioridazine-once a common treatment-was pulled from the U.S. market in 2005 because it prolonged QT by up to 35 ms on average. It’s the worst offender.
- Haloperidol and ziprasidone are moderate to high risk. Haloperidol adds about 4-6 ms, but in people with other risk factors, that’s enough to push QTc over 500 ms.
- Quetiapine and risperidone sit in the middle, with about 5-10 ms prolongation.
- Lurasidone and aripiprazole are among the safest, with lurasidone showing almost no effect in large studies.
Cardiac Medications Make the Risk Worse
This isn’t just about antipsychotics alone. The real danger often comes from combining them with other drugs that also prolong the QT interval. Think of it like stacking weights on a scale-each one adds pressure. Common cardiac medications that can interact include:- Antiarrhythmics like amiodarone and sotalol
- Antibiotics like moxifloxacin and erythromycin
- Antifungals such as fluconazole
- Some antidepressants, including citalopram and escitalopram
Who’s Most at Risk?
Some people are more vulnerable than others, even with the same medication. Risk factors stack up:- Age over 65-risk doubles
- Female sex-women are 1.7 times more likely to develop QT prolongation
- Low potassium or magnesium-levels below 3.5 mmol/L for potassium increase risk by 28%
- Heart disease-especially prior arrhythmias or heart failure
- High doses-risk increases with dose, not just drug choice
- Genetics-some people have inherited conditions like Long QT Syndrome that make them far more sensitive
How Doctors Monitor and Manage the Risk
It’s not about avoiding antipsychotics-it’s about managing them safely. Here’s what works:- Baseline ECG-before starting any antipsychotic, especially high-risk ones.
- Repeat ECG within one week of reaching a stable dose. This catches most of the prolongation early.
- Annual ECGs for anyone on long-term therapy.
- Check electrolytes-potassium should be above 4.0 mmol/L, magnesium above 1.8 mg/dL.
- Review all medications-including over-the-counter and herbal ones. Even some cough syrups can prolong QT.
- Switch to lower-risk drugs if QTc rises above 500 ms or increases by more than 60 ms.
The Big Picture: Benefits vs. Risks
It’s easy to focus on the danger. But here’s the truth: not taking antipsychotics can be deadlier. People with schizophrenia have a 5% lifetime risk of suicide and a 12% higher risk of accidental death. Studies show those who take antipsychotics have 40% lower overall mortality than those who don’t. The mortality curve is U-shaped: people who take no medication and those on very high doses have the worst outcomes. The sweet spot? Low to moderate doses, carefully monitored. Dr. David M. Taylor, a leading expert, says it plainly: "Assume all antipsychotics carry an increased risk of sudden cardiac death. But they also protect against the consequences of schizophrenia."What’s Changing in 2025?
The rules are getting stricter-and smarter.- The FDA now requires thorough QT (TQT) studies for every new antipsychotic, testing on 100+ healthy volunteers.
- European regulators rejected three new antipsychotics between 2015 and 2020 because of cardiac risk.
- 63% of U.S. academic hospitals now have formal QT risk-based prescribing protocols.
- Sales of lurasidone grew 14.2% in 2022, while haloperidol sales dropped 3.7%-doctors are choosing safer options.
- Telemedicine ECGs are becoming common, making monitoring easier in rural or community settings.
What You Can Do
If you or someone you care for is on an antipsychotic:- Ask for a baseline ECG before starting.
- Ask if your drug is high, moderate, or low risk.
- Get your potassium and magnesium checked if you’re on diuretics or have poor appetite.
- Bring a full list of all medications-prescription, OTC, supplements-to every appointment.
- Don’t skip follow-up ECGs. They’re not optional.
- If you feel dizzy, faint, or have palpitations, get checked immediately.
Can antipsychotics cause sudden death?
Yes, in rare cases. The main danger is QT prolongation leading to torsade de pointes, a life-threatening heart rhythm. This risk is highest with certain drugs like thioridazine and haloperidol, especially when combined with other QT-prolonging medications or in people with low potassium, heart disease, or older age. But the overall risk is low when monitored properly. Studies show the benefit of antipsychotics in reducing suicide and accidental death far outweighs the cardiac risk for most patients.
Which antipsychotic is safest for the heart?
Lurasidone is currently the safest option based on clinical data, with minimal QT prolongation (close to zero in most studies). Aripiprazole, brexpiprazole, and paliperidone also carry very low risk. Haloperidol and ziprasidone are higher risk, and thioridazine is no longer available in the U.S. due to its danger. Always ask your doctor which drug fits your heart profile.
Do I need an ECG if I’m on a low-risk antipsychotic?
Yes, still. Even low-risk drugs can cause prolongation if you have multiple risk factors-like being over 65, female, low potassium, or taking other medications that affect the heart. Guidelines recommend a baseline ECG before starting any antipsychotic, and a repeat one within a week of reaching your full dose. Annual checks are advised for long-term users.
Can I stop my antipsychotic if I’m worried about my heart?
Never stop abruptly. Stopping antipsychotics suddenly can cause rebound psychosis, severe agitation, or even suicide. If you’re concerned about heart risks, talk to your doctor. They can check your ECG, test your electrolytes, and switch you to a safer medication if needed. The goal is not to avoid treatment-it’s to make it safer.
How do I know if my QT interval is too long?
You can’t tell by symptoms alone. Many people with prolonged QT feel nothing until they faint or have cardiac arrest. The only way to know is through an ECG. A corrected QT interval (QTc) over 500 ms is dangerous. An increase of more than 60 ms from your baseline is also a warning sign. Your doctor should review your ECGs and compare them over time.
Are there alternatives to antipsychotics for psychosis?
For severe psychosis, antipsychotics are the most effective treatment. Non-drug options like cognitive behavioral therapy (CBT) can help with symptoms but are not substitutes for medication in acute or chronic cases. Some newer treatments like transcranial magnetic stimulation (TMS) are being studied, but they’re not yet standard. The key is choosing the right antipsychotic with the lowest cardiac risk-not avoiding treatment altogether.






Jane Lucas
December 29, 2025 AT 03:54i just started on lurasidone last month and my dr said my qt was fine but i still panic every time i feel my heart skip... like is it just anxiety or is it actually happening?? idk but im glad theyre testing this stuff now
dean du plessis
December 29, 2025 AT 06:30this is the kind of info every patient needs but never gets. most docs just hand you a script and say dont worry about it. but when your heart starts acting weird and you google it you end up in a spiral. thanks for laying it out like this
Anna Weitz
December 29, 2025 AT 08:15people act like antipsychotics are some evil magic pill but the real villain is the system that pushes high risk meds because theyre cheap and insurance wont cover the safer ones
Elizabeth Alvarez
December 29, 2025 AT 11:04you know what they dont tell you the pharmaceutical companies have been hiding the cardiac data for decades they run these so called clinical trials but they cherry pick the data and bury the deaths if you dig deep enough youll find internal memos from the 90s where they called ziprasidone a walking time bomb and still pushed it because the profits were too good and now theyre pushing lurasidone like its a miracle drug but wait till the next side effect emerges its always the same playbook they make money off your fear and your illness and then they sell you the fix that costs 800 a month and dont even get me started on the ECG monitoring being a billing loophole for hospitals
Miriam Piro
December 31, 2025 AT 01:02the truth is we live in a world where your mind is policed by your heart 🤡 and if your heart doesnt behave the way the algorithm says it should you get labeled high risk and stripped of your autonomy. they monitor your QT interval like its a stock ticker and if it dips below 500 ms you get flagged as a liability not a person. we dont need more ECGs we need a system that sees us as human not a risk profile. the real torsade de pointes is the one in the boardroom where the shareholders vote on your survival
John Barron
December 31, 2025 AT 05:20It is imperative to underscore that the pharmacokinetic interactions between antipsychotics and QT-prolonging agents constitute a clinically significant pharmacodynamic synergy that elevates the risk of ventricular arrhythmogenesis. Furthermore, the presence of comorbid hypokalemia and advanced age constitutes a triad of risk factors that exponentially increases mortality potential. I strongly recommend that all clinicians adhere to the CredibleMeds classification system and implement mandatory baseline and follow-up ECGs as per ACC/AHA guidelines. Failure to do so constitutes a breach of the standard of care.
Nicola George
December 31, 2025 AT 12:51so you're telling me the same drugs that keep me from screaming at the ceiling are the ones that might stop my heart? cool. so what's the alternative? die quietly or die with a monitor on? 🤷♀️
Kylie Robson
December 31, 2025 AT 19:02the QTc correction formula is flawed in real-world populations due to Bazett's overcorrection at high heart rates and undercorrection at low rates. Recent meta-analyses suggest Fridericia's formula is more accurate for psychiatric populations on polypharmacy. Also, don't forget the role of CYP2D6 polymorphisms in haloperidol metabolism-poor metabolizers have 3x higher plasma concentrations. This is why pharmacogenomic testing should be standard before initiating any high-risk antipsychotic.