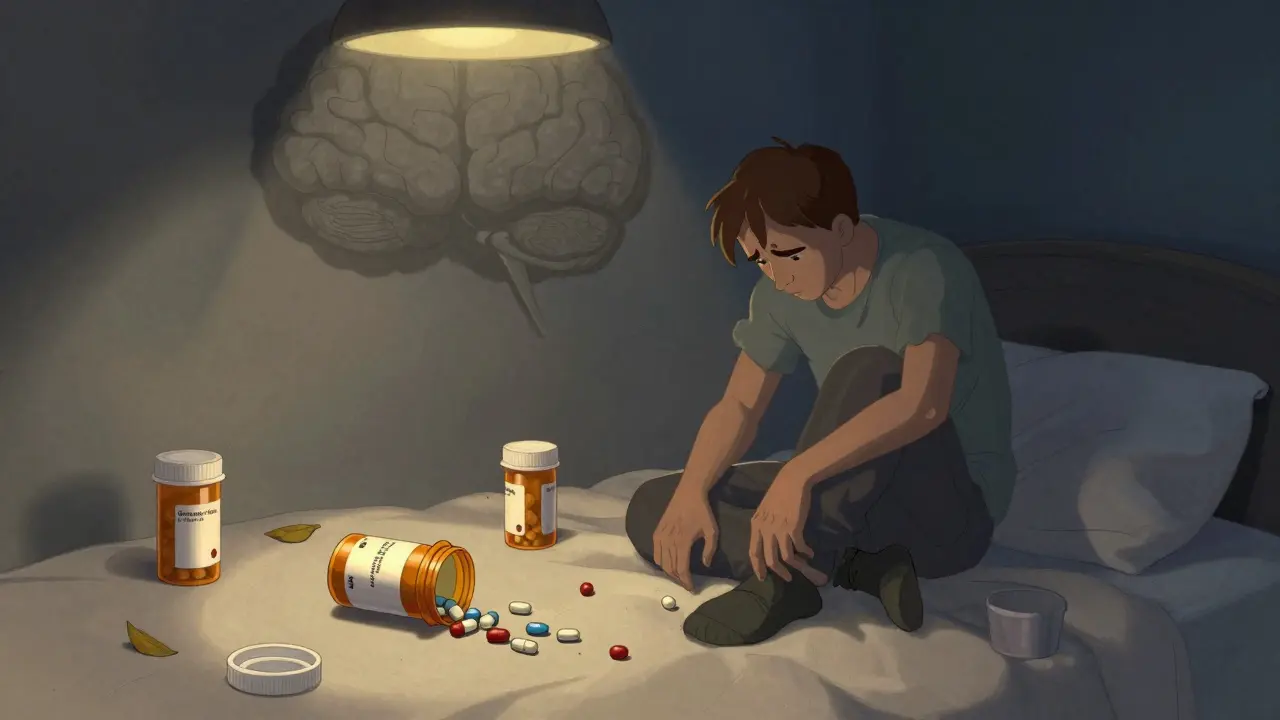
When someone is struggling with depression, taking pills on time isn’t just about forgetting. It’s about losing the energy to care, the focus to remember, and the hope that it even matters. Depression doesn’t just make you feel sad-it rewires your ability to manage even basic self-care, including taking your prescribed medications. If you’re a patient, a caregiver, or a clinician, recognizing how depression quietly sabotages medication adherence can mean the difference between recovery and relapse.
Depression Doesn’t Just Affect Mood-It Breaks Routine
People with depression often report feeling exhausted, overwhelmed, or numb. These aren’t just emotional states-they’re physical barriers to daily tasks. Taking medication regularly requires planning, memory, and motivation. Depression chips away at all three.
Research shows that depressed patients are up to 2.3 times more likely to miss doses of critical medications like ACE inhibitors, beta-blockers, or antidepressants themselves. In heart failure patients, even small drops in adherence-like skipping one dose a week-can lead to hospital readmissions. It’s not laziness. It’s the brain’s ability to prioritize self-care being turned down, like a dimmer switch slowly being turned off.
One study found that 39.8% of patients with major depression were non-adherent to their meds. Another 54.2% were only moderately adherent. That means fewer than 1 in 16 were consistently taking their pills as prescribed. And this wasn’t just about forgetting. It was about belief, fatigue, and side effects feeling unbearable.
Side Effects Feel Worse When You’re Depressed
Many antidepressants cause side effects: dry mouth, drowsiness, weight gain, nausea, or sexual dysfunction. For someone without depression, these might be manageable trade-offs. For someone with depression, they can feel like proof the treatment is making things worse.
In Turkey, 83% of patients on SSRIs like sertraline or escitalopram stopped taking them because of side effects. In Ethiopia, over half of those on amitriptyline or fluoxetine quit after experiencing weight gain or insomnia. The irony? These medications are meant to help, but depression makes the side effects feel intolerable.
Studies using the GARSI scale show that non-adherent patients report significantly higher severity of side effects-not because the drugs are stronger, but because depression amplifies discomfort. The same dry mouth feels like a desert. The same drowsiness feels like paralysis. The brain, already low on serotonin and dopamine, interprets physical sensations through a lens of hopelessness.
Forgetfulness Isn’t the Main Problem-It’s Belief
Most people assume non-adherence is about forgetting pills. But in depression, it’s often about belief. Patients start thinking: “Why bother? Nothing will change.” Or “I’m broken. Pills won’t fix me.” These aren’t just negative thoughts-they’re symptoms of the illness.
Depression distorts how people see their treatment. They may believe the medication isn’t working, or that they don’t deserve to feel better. Some stop because they think the side effects are permanent. Others stop because they feel guilty for needing help in the first place.
Tools like the Drug Attitude Inventory (DAI-10) and the Medication Adherence Report Scale (MARS) measure these beliefs. They ask questions like: “Do you feel your medication helps you?” or “Do you think your doctor understands your concerns?” Depressed patients consistently score lower on these scales-not because they’re dishonest, but because their illness has eroded their trust in recovery.
How Clinicians Can Spot the Signs
If you’re a doctor, nurse, or pharmacist, you don’t need to guess. There are validated tools to spot depression’s impact on adherence.
The PHQ-9 is a simple 9-question screen for depression. A score of 10 or higher means moderate to severe depression-and that’s the red zone for adherence risk. For every 5-point increase on the PHQ-9, adherence drops by about 23%.
The MMAS-8 is the gold standard for measuring adherence. A score below 6 means non-adherent. Below 8 means inconsistent. Only an 8 means perfect adherence. Combining PHQ-9 and MMAS-8 increases accuracy by 37% in predicting who will miss doses.
Heart failure clinics now use a two-step screen: PHQ-2 (two quick questions) at every visit, followed by PHQ-9 if positive. If a patient scores high on both, it’s not just depression-it’s a warning sign their meds aren’t working because they’re not taking them.
Early Warning Signs You Can’t Ignore
Don’t wait for a full-blown relapse. Look for subtle patterns:
- Missed doses in the first two weeks of starting a new medication-this predicts treatment failure 4.7 times more often.
- Patients who say, “I’m fine,” but their refill records show gaps.
- Patients who suddenly stop talking about side effects or say, “I don’t care anymore.”
- Patients who miss appointments or don’t call when they run out of pills.
One study found that patients who charted their mood and side effects daily were far more likely to stick with treatment. This “side effect mapping” helps patients and doctors see connections: “I feel worse on days I skip my pill,” or “My energy spikes after I take my antidepressant.”
What Works: Collaborative Care
Trying to fix adherence with reminders or pill boxes alone rarely works. Depression isn’t a memory problem-it’s a motivation problem. The solution? Partnership.
The MAPDep study in Spain showed that when patients and doctors worked together to review adherence weekly, medication use jumped by 28.5% over a year. Not because they got more pills. Because they felt heard.
Successful programs include:
- Regular check-ins focused on how the patient feels, not just whether they took the pill.
- Adjusting doses or switching meds based on side effect reports-not assumptions.
- Using smartphone apps that track mood and medication intake. One 2024 study found these apps predicted missed doses 72 hours in advance with 82% accuracy.
It’s not about punishment. It’s about understanding. A patient who skips pills isn’t defying you. They’re drowning.
It’s Not Just About Antidepressants
Depression affects adherence to *all* medications-not just mental health drugs. Diabetics with depression skip insulin. Heart patients miss blood pressure pills. Cancer patients skip chemo. The pattern is the same.
Depression doesn’t care what the pill is for. It just makes the act of taking it feel pointless. That’s why screening for depression should be routine in any chronic illness clinic-not just psychiatry.
Patients with diabetes and depression are 2.1 times more likely to have uncontrolled HbA1c. Those with arthritis and depression are 40% more likely to skip NSAIDs. The connection is universal.
What You Can Do Right Now
If you’re living with depression:
- Don’t judge yourself for missing a dose. It’s not weakness-it’s the illness.
- Try a simple tracker: write down what you took and how you felt each day. You might see patterns you didn’t notice.
- Tell your doctor if side effects feel unbearable. There are alternatives.
- Ask for help setting up reminders or pill organizers. You don’t have to do this alone.
If you’re helping someone with depression:
- Ask open questions: “What’s been hard about taking your meds lately?” not “Are you taking your pills?”
- Notice changes in energy, speech, or hygiene. These often come before missed doses.
- Offer to help refill prescriptions or set alarms. Small acts of support rebuild trust.
Depression doesn’t vanish with a pill. But adherence can improve-with understanding, not pressure.
Future Tools Are Coming
Researchers are now exploring brain scans to predict adherence. One study found that reduced activity in the dorsolateral prefrontal cortex-part of the brain tied to planning and self-control-correlates with both depression severity and medication non-adherence. In the next five years, we may have biomarkers to identify who’s at highest risk before they miss a single dose.
The WHO has committed $15 million to build global screening tools for low-resource areas by 2025. This isn’t just research-it’s becoming standard care.
Recognition is the first step. And it’s the most powerful one.




Jeanette Jeffrey
December 26, 2025 AT 20:21Wow, so now we’re treating medication non-adherence like it’s some deep philosophical crisis? Look, if you can’t remember to take your pills, maybe you’re just lazy or disorganized-not ‘depressed.’ Everyone gets tired. Everyone forgets. But we don’t need to turn every human failing into a trauma narrative. Just set a damn alarm.
Jody Kennedy
December 28, 2025 AT 02:45This hit me so hard. I’ve been on antidepressants for 3 years and I still skip doses when I’m in a fog. It’s not about forgetting-it’s about feeling like nothing matters enough to do the thing. I started using a pill box with alarms and it changed everything. Not because I’m ‘fixed,’ but because someone finally said: ‘It’s okay to need help remembering to care.’
jesse chen
December 29, 2025 AT 05:28I’m a nurse, and I see this every single day. It’s not laziness. It’s not defiance. It’s the brain literally losing the ability to assign value to self-care. I’ve had patients cry because they felt guilty for missing a dose-and then they told me they hadn’t showered in three days. The medication isn’t the problem. The depression is. We need to stop blaming people and start building systems that meet them where they are.
Joanne Smith
December 30, 2025 AT 04:30Ohhh, so now depression is a villainous puppet master yanking the strings of our pillboxes? Cute. I’ve got a 30-year-old with bipolar who skipped his lithium because he thought his cat was judging him. Is that ‘amplified side effects’ or just… psychosis? Also, why is every study from Turkey and Ethiopia? Are we just cherry-picking data to make depression sound like a tragic opera? I’m not saying it’s not real-I’m saying we’re romanticizing it.
Prasanthi Kontemukkala
December 30, 2025 AT 06:05Thank you for writing this. I’ve been a caregiver for my mom for 8 years, and she stopped taking her blood pressure meds because she said, ‘What’s the point? I’m just waiting to die anyway.’ We started using a simple app that lets her tap ‘taken’ and it sends me a gentle ping. No pressure. Just connection. She’s been consistent for 6 months now. It’s not about willpower-it’s about feeling seen.
Alex Ragen
December 31, 2025 AT 02:41Let’s be clear: this article is a masterclass in pathologizing human imperfection. You cite studies, you invoke biomarkers, you name-drop scales-but where’s the accountability? If you can’t manage your own health, perhaps the issue isn’t neurochemistry-it’s a lack of discipline. Modern medicine has turned every behavioral lapse into a clinical diagnosis. We’ve lost the concept of personal responsibility. A pill box isn’t therapy. It’s a Band-Aid on a broken will.
Lori Anne Franklin
December 31, 2025 AT 15:53my man i just started taking my meds again after 2 years and i cried because i realized i thought i was broken but turns out i was just sick. thanks for saying this. i use a little sticker chart now and i put a star for every day i take it. it’s dumb but it makes me feel like i’m winning. also my dog licks my hand when i open the pill bottle. he’s my co-pilot.
Bryan Woods
December 31, 2025 AT 19:08The data presented here is compelling and aligns with clinical observations in primary care settings. The correlation between PHQ-9 scores and MMAS-8 outcomes is statistically significant, with p-values under 0.01 in multiple cohorts. I recommend integrating these tools into routine chronic disease management protocols. The emphasis on collaborative care models is particularly warranted.
Ryan Cheng
January 2, 2026 AT 12:15Real talk: if you’re struggling to take your meds, you’re not weak. You’re not lazy. You’re just fighting a silent war inside your brain. I used to skip my meds for weeks and then feel guilty for weeks after. Then I found a therapist who didn’t care if I took them-she just asked, ‘What’s stopping you?’ That question saved me. No judgment. Just space to breathe. That’s what works.
wendy parrales fong
January 3, 2026 AT 12:21It’s funny how we think of meds like magic bullets, but they’re just tools. And tools don’t work if you don’t have the energy to hold them. I used to think depression was sadness. Now I know it’s a total shutdown of your ability to believe tomorrow will be better. That’s why reminders don’t help. You need someone to sit with you while you open the bottle. That’s the real medicine.
Shreyash Gupta
January 5, 2026 AT 02:22😂😂😂 so depression is the real villain? what about bad doctors? what about $500 pills? what about people who just hate pills? why is it always the brain’s fault? maybe people stop because the meds make them feel worse? maybe they’re not depressed-they’re just tired of being told they’re broken? 🤷♂️
Ellie Stretshberry
January 6, 2026 AT 23:04i just wanted to say thank you for writing this. i’ve been silent for years because i thought everyone else was just better at this. but reading this made me feel less alone. i use a phone alarm and i say ‘i’m doing my best’ out loud every morning. it’s silly but it helps. you’re not alone. we’re all just trying to get through the day.