Chest Congestion & Sleep Apnea Risk Checker
Assess Your Symptom Overlap
Select symptoms you experience to determine potential connection between chest congestion and sleep apnea.
Nighttime Symptoms
Daytime Symptoms
When you notice Chest Congestion is a buildup of mucus or fluid in the lungs and airways that makes breathing feel heavy or blocked, you might think it’s just a cold. But it can also set the stage for Sleep Apnea, a sleep‑related breathing disorder where breathing stops briefly during sleep.
chest congestion isn’t always a headline problem, yet its link to nighttime breathing issues is surprisingly strong. In this guide we’ll unpack why this happens, what signs to watch for, and how to keep both conditions in check.
What Is Chest Congestion?
Mucus is a sticky, gel‑like secretion that lines the respiratory tract to trap dust, microbes and other irritants is the main culprit behind chest congestion. When infection, allergies, or irritants cause excess mucus, the airways swell - a condition known as Airway Inflammation is the swelling and irritation of the bronchial tubes that narrows the passage for air. This narrowing makes it harder for air to move in and out, especially when you lie down.
Common triggers include colds, flu, bronchitis, asthma flare‑ups, and even chronic conditions like GERD gastro‑esophageal reflux disease, where stomach acid backs up into the throat, irritating the airways. The result is a feeling of tightness, coughing, and the classic “phlegmy” sound during deep breaths.
Understanding Sleep Apnea
Sleep apnea comes in two main flavors. Obstructive Sleep Apnea (OSA) occurs when soft tissue in the throat collapses during sleep, blocking the airway is the most common type. Central Sleep Apnea happens when the brain fails to send proper signals to the muscles that control breathing is rarer but can coexist with OSA.
Both types lead to brief pauses in breathing-usually lasting 10 to 30 seconds-followed by a gasp or choking sound as oxygen levels dip. Over time, the repeated drops in oxygen can raise blood pressure, strain the heart, and cause daytime fatigue.
Why Chest Congestion Can Set Off Sleep Apnea
The connection hinges on three simple mechanisms:
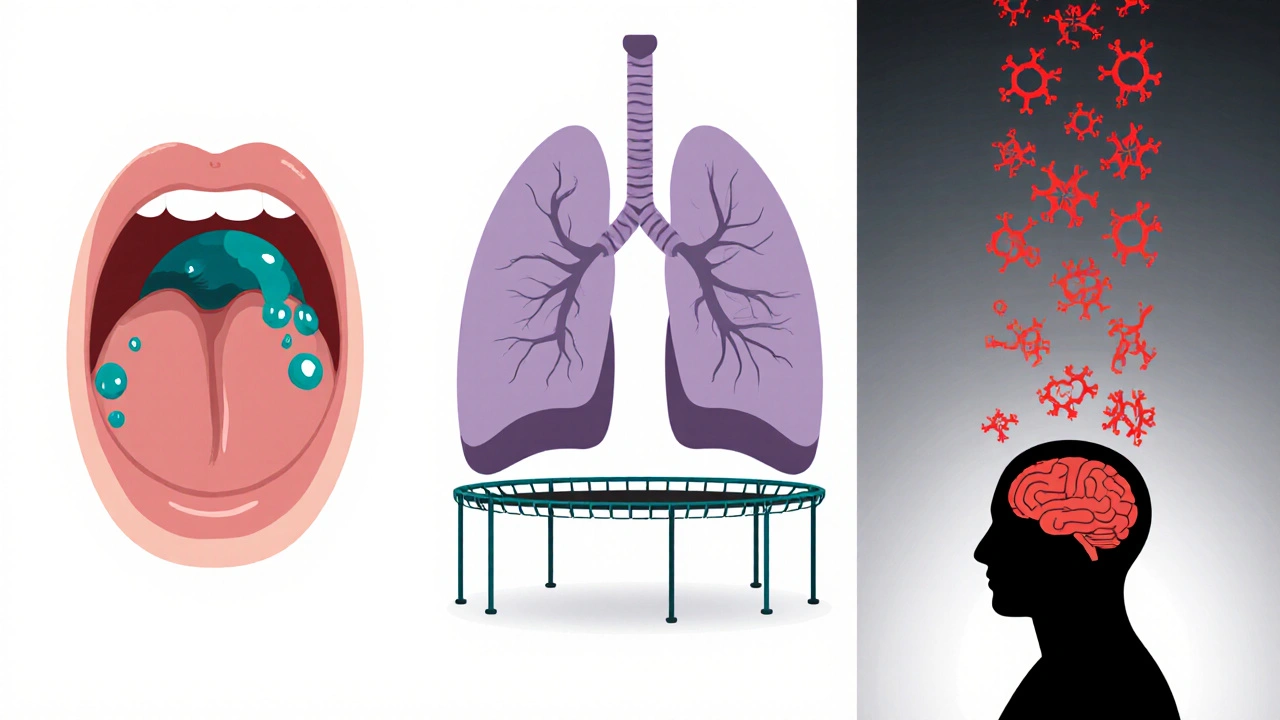
- Nasal and Upper‑Airway Blockage: Excess mucus drips down the throat (post‑nasal drip) and swells the soft palate. This adds extra bulk to the area that already tends to collapse during sleep, making OSA more likely.
- Reduced Lung Volume: When the lungs can’t fully expand because of congestion, the chest wall’s “support” for the airway drops. Think of it as a trampoline losing tension-the airway sags more easily.
- Inflammatory Cascade: Inflammation releases cytokines that affect the nervous system’s control of breathing. This can tip the balance toward central sleep apnea in vulnerable individuals.
Research from the American Thoracic Society (2024) found that people with chronic bronchitis reported a 38% higher incidence of OSA compared to those without respiratory symptoms. The study highlighted mucus‑related airway narrowing as a key driver.
Spotting the Overlap: Symptoms to Watch For
Because chest congestion and sleep apnea share some signs, it’s easy to miss the overlap. Here’s a quick checklist to differentiate and spot the combo:
- Persistent coughing at night that wakes you up.
- Waking up with a dry, sore throat or a “gurgling” sound.
- Loud snoring that intensifies after a cold or flu.
- Morning headaches - a classic sign of low oxygen during sleep.
- Daytime fatigue that doesn’t improve with coffee.
- Chest tightness that feels worse when you lie flat.
If you tick more than half of these, it’s worth discussing both conditions with a healthcare professional.
Diagnosing the Duo
Doctors use a combination of tools:
- Physical Exam: Listening for wheezes, checking throat size, and assessing nasal passages.
- Sleep Study (Polysomnography): Overnight monitoring of breathing, oxygen levels, and brain activity. It’s the gold standard for confirming sleep apnea.
- Chest X‑ray or CT Scan: To see fluid buildup, lung inflammation, or structural issues.
- Spirometry: Measures airflow and can reveal chronic obstructive pulmonary disease (COPD) that often co‑exists with congestion.
In many clinics, a home sleep‑apnea test (HSAT) is also available, letting patients wear a small device for a night at home while the data is uploaded for analysis.
Treatment Strategies That Hit Both Targets
Effective management means tackling mucus production, airway inflammation, and the apnea itself. Below are the main options, grouped by category.
1. Clearing the Airway
- Hydration: Drinking plenty of water thins mucus, making it easier to cough up.
- Steam Inhalation: A hot shower or a bowl of steaming water (add a few drops of eucalyptus oil) can loosen secretions.
- Expectorants: Over‑the‑counter medicines like guaifenesin boost mucus clearance.
- Nasal Saline Rinses: Using a neti pot or squeeze bottle clears post‑nasal drip and reduces swelling.
2. Reducing Inflammation
- Inhaled Corticosteroids: Common for asthma, they shrink airway walls and lower mucus production.
- Anti‑histamines: Helpful if allergies trigger congestion.
- Dietary Tweaks: Cutting down on dairy, fried foods, and sugar can lower mucus thickness for some people.
3. Direct Sleep Apnea Therapies
- Continuous Positive Airway Pressure (CPAP): CPAP delivers a steady stream of pressurized air through a mask to keep the airway open during sleep. It’s the most effective first‑line treatment for OSA.
- Bi‑Level Positive Airway Pressure (BiPAP): Adjusts pressure for inhalation and exhalation, useful for people who find CPAP uncomfortable.
- Oral Appliances: Custom‑made devices that reposition the lower jaw and tongue.
- Positional Therapy: Encouraging side‑sleeping with pillows or specialized belts.
- Surgery: Procedures like uvulopalatopharyngoplasty (UPPP) remove excess tissue, but are usually last‑resort.
4. Lifestyle Adjustments
- Weight Management: Extra neck fat squeezes the airway. Even a 5‑10% weight loss can lower apnea severity.
- Alcohol & Sedatives: Limit intake before bed; they relax throat muscles, worsening obstruction.
- Regular Exercise: Boosts lung capacity and reduces systemic inflammation.
- Elevated Sleeping Position: Raising the head of the bed 4‑6 inches helps mucus drain and keeps the airway open.
Quick Reference Table
| Aspect | Chest Congestion | Sleep Apnea |
|---|---|---|
| Primary Cause | Mucus buildup, airway inflammation | Airway collapse (OSA) or brain signal loss (central) |
| Typical Symptoms | Cough, phlegm, wheeze, chest tightness | Loud snoring, gasping, daytime sleepiness |
| Night‑time Impact | Worsens when lying flat, may trigger awakenings | Breathing pauses, oxygen dips, fragmented sleep |
| Common Triggers | Colds, flu, allergies, GERD | Obesity, alcohol, sedatives, nasal blockage |
| Key Treatments | Hydration, expectorants, steroids, nasal rinses | CPAP/BiPAP, oral devices, weight loss, surgery |
| Potential Overlap | Post‑nasal drip adds bulk to throat, raising risk of OSA | Apnea can worsen nighttime cough by causing dry mouth |
When to Seek Professional Help
If you notice any of these red‑flag signs, schedule an appointment promptly:
- Breathing pauses lasting longer than 20 seconds. \n
- Persistent morning headaches or dry mouth.
- Sudden weight gain combined with louder snoring.
- Chest pain or shortness of breath at rest.
Early detection can prevent long‑term complications like hypertension, heart disease, and chronic fatigue.
Pro Tips to Keep Both Conditions in Check
- Track Your Sleep: Use a smartphone app or wearable to note snoring intensity and nighttime cough frequency.
- Seasonal Allergy Prep: Start antihistamines a week before pollen peaks to keep mucus low.
- Upgrade Your Pillow: A hypoallergenic, firm pillow supports neck alignment and reduces airway collapse.
- Mind the Air Quality: A HEPA filter or humidifier can trim irritants that trigger congestion.
- Regular Check‑ups: Annual lung function tests catch early inflammation before it spirals.
Bottom Line
Chest congestion isn’t just an annoying cough; it can be a silent catalyst for sleep apnea. By recognizing the overlap, treating the mucus, and addressing airway health, you can protect your sleep quality and overall well‑being. If you suspect the two are linked in your case, talk to a doctor about a sleep study and a targeted respiratory plan.
Frequently Asked Questions
Can chest congestion cause sleep apnea?
Yes. Excess mucus and airway swelling can add bulk to the throat, increasing the chance that the airway collapses during sleep, especially in people already prone to obstructive sleep apnea.
What’s the fastest way to clear mucus before bedtime?
A warm steam inhalation combined with a saline nasal rinse works within minutes. Follow up with a glass of water and an over‑the‑counter expectorant if needed.
Is CPAP safe for someone with chronic bronchitis?
CPAP is generally safe and can actually help by keeping airways open, which reduces mucus pooling. Your doctor may adjust humidity settings on the machine to keep airways moist.
Do allergies worsen sleep apnea?
Allergic inflammation swells nasal passages and the soft palate, making airway collapse more likely. Treating allergies often improves both snoring and apnea severity.
Can weight loss reduce both congestion and apnea?
Losing excess neck fat can open the airway, while a lighter body reduces overall inflammation, which may cut down mucus production. Even modest weight loss (5‑10%) often shows measurable improvement.







Rohit Sridhar
October 17, 2025 AT 19:30Great breakdown! I’ve seen many patients dismiss chest congestion as just a cold, only to end up with nighttime breathing struggles. Keeping the airway clear before bed really makes a difference, especially with a simple steam inhalation and saline rinse. Pair that with a short walk after dinner to boost lung capacity, and you’ll notice less snoring and fewer wake‑ups. If you can, track your symptoms in a sleep app – the patterns become crystal clear. Stay motivated, and don’t let a stubborn cough ruin your REM cycles!
kendra mukhia
October 19, 2025 AT 13:10Listen up, because the link between mucus and apnea is not some myth that the internet conjures on a lazy Tuesday.
When your chest is clogged, the diaphragm loses its spring, and the airway becomes a sagging hammock for the night.
That sagging hammock is exactly what collapses under the weight of swollen tissue, turning a simple cough into a full‑blown apnea episode.
Studies from the American Thoracic Society clearly show a 38% increase in OSA among chronic bronchitis sufferers, and that is not a rounding error.
The inflammatory cascade releases cytokines that mess with the brain’s respiratory centers, effectively turning off the automatic breathing switch.
If you think a little post‑nasal drip is harmless, think again – it adds bulk to the soft palate, creating a perfect storm for obstruction.
Moreover, reduced lung volume means less negative pressure to keep the airway taut, so the walls collapse like a deflated balloon.
Even a modest weight gain can amplify this effect, because extra neck fat squeezes the airway from the outside.
And let’s not forget GERD; acid reflux can inflame the upper airway, making the whole situation worse than a double‑header of bad news.
The good news is that you can fight back with a multi‑pronged approach: hydration, steam, nasal rinses, and-yes-CPAP with humidification.
A well‑adjusted CPAP not only splints the airway open but also pushes out excess mucus, reducing the choking episodes.
Don’t dismiss over‑the‑counter expectorants; guaifenesin thins the mucus, making it easier for the body to clear it before you lie down.
If you’re allergic, a daily antihistamine can shrink that swollen palate, shaving minutes off your apnea index.
And for the long haul, consider lifestyle tweaks: lose that extra five to ten percent weight, limit alcohol, and keep your head elevated while you sleep.
Bottom line: treat the congestion aggressively, and you’ll see a dramatic drop in apnea events-no magic, just science.
Sarah Hanson
October 21, 2025 AT 04:03Thank you for the thorough overview; the integration of airway clearance and CPAP settings is particularly valuable. I definately recommend patients track nightly symptom changes to inform their treatment plan.
Wyatt Schwindt
October 22, 2025 AT 16:10Tracking cough frequency with a sleep app can highlight patterns without needing a full polysomnography.
Bethany Torkelson
October 24, 2025 AT 01:30Stop ignoring chest congestion; it’s a direct trigger for sleep apnea and must be treated now.
Natala Storczyk
October 25, 2025 AT 08:03Wake up, America!!! The silent epidemic of mucus‑induced apnea is ruining our nation’s health!!! Only a fierce, united fight against congestion will save our sleep and our future!!!
Avril Harrison
October 26, 2025 AT 10:50It's wild how something as simple as a runny nose can mess with your snooze, but a warm tea and a good pillow can work wonders.
nitish sharma
October 27, 2025 AT 11:50I concur with the observations; implementing humidifiers and proper sleep positioning provides a pragmatic solution that aligns with the clinical recommendations outlined earlier.