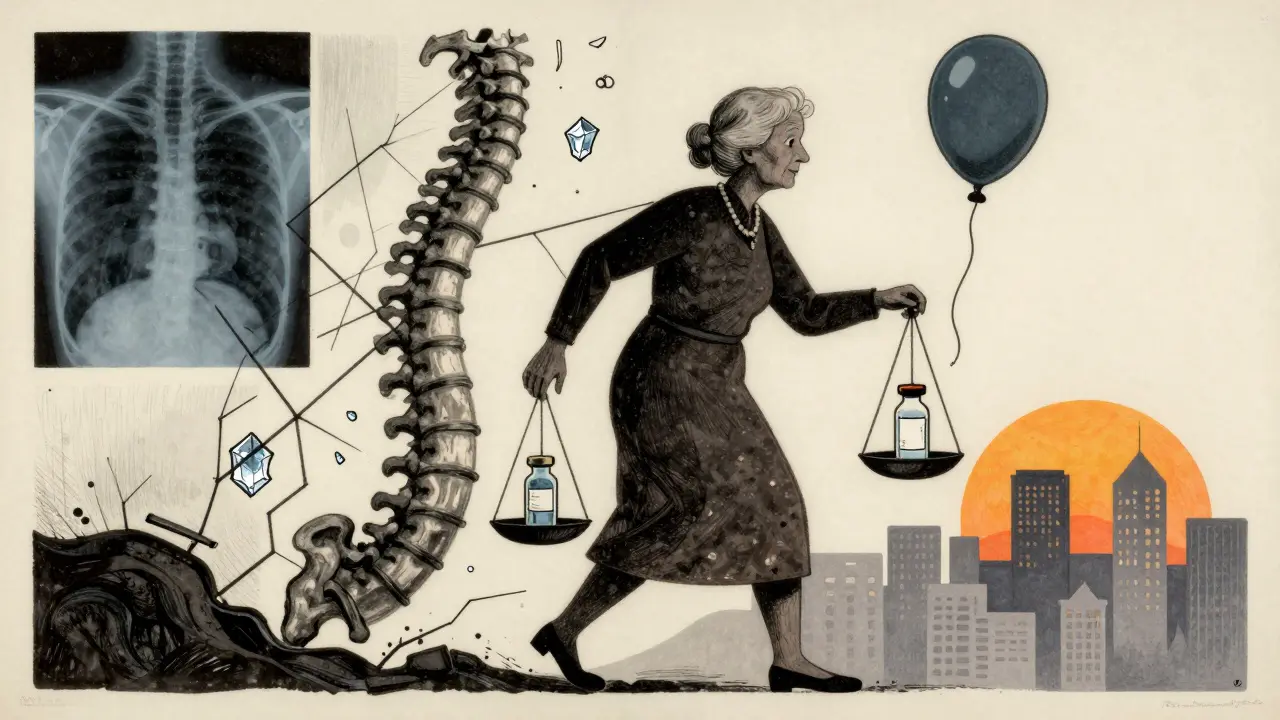
When your spine hurts from a broken vertebra, what can actually help?
If you’ve been told you have a vertebral compression fracture-especially if it’s from osteoporosis-you’re not alone. Around 700,000 people in the U.S. suffer these fractures every year. Most are over 65, and women are far more likely to be affected. The pain can be crushing, literally. Standing, walking, even breathing becomes hard. And if you’ve tried rest, painkillers, or a back brace for weeks with no real improvement, you might be wondering: is there something faster, something that actually works?
That’s where kyphoplasty and vertebroplasty come in. Both are minimally invasive procedures designed to stop the pain and stabilize your spine. They’re not surgery in the traditional sense-no big cuts, no long hospital stays. Most people go home the same day. But they’re not the same. And knowing the difference could mean the difference between a quick fix and a lasting change.
How do kyphoplasty and vertebroplasty actually work?
Both procedures use the same end goal: inject medical-grade bone cement into the fractured vertebra. The cement hardens in 10 to 20 minutes, acting like an internal cast that holds the bone together. The difference is in how they get there.
Vertebroplasty is simpler. A thin needle is guided through your skin and into the broken bone using real-time X-ray imaging. Then, cement is injected directly into the fracture under pressure. The cement spreads through the spongy inner bone, locking the pieces in place. It takes about 30 to 60 minutes. You’re awake but sedated. Most people feel pain relief within hours.
Kyphoplasty adds a step. Before the cement goes in, a small balloon is inserted through the same needle. It’s inflated with saline to gently lift the collapsed bone back toward its normal height. Think of it like propping up a squashed soda can. Once the balloon is deflated and removed, it leaves a cavity. Then, the cement is injected into that space under lower pressure. This reduces the chance of cement leaking out where it shouldn’t.
That extra balloon step is why kyphoplasty takes a bit longer-usually 45 to 75 minutes. But it’s also why it’s preferred when the fracture has caused visible deformity, like a hunched back (kyphosis). Vertebroplasty doesn’t try to fix the shape. Kyphoplasty does.
Which one gives better pain relief?
Here’s the surprising part: both procedures work about equally well for pain.
Studies show 85% to 90% of patients report immediate pain relief after either procedure. Before treatment, average pain scores on a scale of 0 to 10 are around 8.2. Within 24 hours, that drops to about 1.5. That’s not just a little better-it’s life-changing. Many patients say it’s like flipping a switch.
One patient on a chronic pain forum described it: “I went from 9/10 pain to 2/10 in hours. I hadn’t slept through the night in months.” Another said, “I didn’t realize how much I was holding my breath until I could breathe normally again.”
There’s no clear winner here. Both deliver rapid, reliable pain relief. So if your main goal is to stop the pain, either option will likely do the job.
What about restoring height and fixing posture?
This is where kyphoplasty shines.
Vertebroplasty doesn’t restore height. The cement fills the space, but it doesn’t lift the bone. If your spine collapsed by 30% or more, you’re still left with a hunched posture after vertebroplasty.
Kyphoplasty, on the other hand, can restore 40% to 60% of the lost height. That’s not just cosmetic. Restoring height reduces pressure on nearby nerves and helps you stand taller. It can also reduce strain on other vertebrae, lowering the risk of future fractures.
But here’s the catch: that restored height doesn’t always last. A 2007 study found that after just 500 daily movements (like walking or standing), about 30% of the height gained slowly settles back down. The bone doesn’t fully heal-it’s stabilized, not rebuilt.
So if your main concern is looking straighter or avoiding a hunched back, kyphoplasty gives you a better shot. But if you’re just trying to stop the pain, vertebroplasty works just as well.

Which is safer? Risk of cement leakage
Cement leakage is the biggest concern with both procedures. If cement leaks out of the bone and into surrounding tissue, it can press on nerves or even travel to the lungs.
With vertebroplasty, leakage happens in 27% to 68% of cases. Most are harmless-seen only on X-rays and causing no symptoms. But about 1.1% of patients have serious complications from it.
Kyphoplasty cuts that risk in half. Leakage occurs in only 9% to 33% of cases. The balloon creates a controlled space for the cement, so it’s less likely to spread where it shouldn’t. Symptomatic complications drop to around 0.6%.
Dr. Steven Cohen from Johns Hopkins says the balloon tamp “reduces cement leakage risk by about 40%,” especially helpful for people with very weak bones from osteoporosis or cancer.
If you’re older, have brittle bones, or your fracture is in a tricky spot, kyphoplasty’s lower leakage rate makes it the safer pick.
Cost difference: Why does it matter?
Kyphoplasty costs 20% to 30% more than vertebroplasty. In 2023, Medicare paid about $3,850 for kyphoplasty and $2,950 for vertebroplasty. That’s a $900 difference per procedure.
That gap exists because kyphoplasty uses a special balloon device made by companies like Medtronic and Stryker. Vertebroplasty just needs a needle and cement-cheaper tools, lower overhead.
Dr. Richard Jensen’s 2019 cost analysis concluded: “For fractures without deformity, vertebroplasty offers better value.” He argues that since both procedures relieve pain equally, paying extra for kyphoplasty doesn’t always make sense.
But if you have significant height loss, kyphoplasty’s added safety and posture benefits may justify the cost. Insurance-especially Medicare-covers both, as long as you’ve tried conservative care first (like bracing, physical therapy, and pain meds for at least 4 to 6 weeks).
Who gets these procedures-and why?
Over 100,000 of these procedures are done in the U.S. every year. About 85% are on people over 65. Women make up 70% to 75% of patients because osteoporosis hits them harder after menopause.
Fractures from trauma (like falls or car accidents) can also be treated this way. So can fractures caused by cancer spreading to the spine.
But not everyone qualifies. If your fracture is old-more than 6 to 8 weeks-and there’s no swelling or inflammation inside the bone (seen on MRI), these procedures won’t help. The cement won’t stick properly. That’s why imaging is so important before you even schedule the procedure.
What’s the recovery really like?
Recovery is fast-by design.
You’ll spend 4 to 6 hours in recovery after the procedure, then go home the same day. You can’t lift anything heavy for 24 hours. Most people walk the same day. Within 72 hours, 92% of patients are back to normal daily activities.
Many stop using opioids within a week. That’s huge. Chronic pain often leads to dependence. These procedures break that cycle.
But there’s a catch: new fractures can happen nearby. About 5% to 10% of patients get another fracture in a different vertebra within a year. That’s not because the procedure failed-it’s because osteoporosis is still there. The cement fixes one bone, but it doesn’t fix the disease.
That’s why follow-up care matters. Calcium and vitamin D supplements. Weight-bearing exercise. Medications like bisphosphonates. Without these, you’re just treating symptoms, not the cause.
What’s new in 2026?
Technology keeps improving. New cement formulas, like calcium phosphate, are being used more often. They’re more like real bone, harden slower, and produce less heat during curing-reducing risk to nearby nerves.
In March 2023, Medtronic got FDA approval for an updated balloon system that’s easier to control and allows more precise height restoration.
And a major 2023 study in The Lancet found that getting treated within two weeks of the fracture cut 12-month mortality by 28%. That’s not just about pain-it’s about survival. Early intervention saves lives.
Right now, kyphoplasty makes up about 65% of these procedures in the U.S. Analysts predict that number will rise to 75% by 2028. Why? Because safety matters. Even if the pain relief is the same, fewer complications mean fewer hospital visits, fewer lawsuits, and better long-term outcomes.
So which one should you choose?
There’s no one-size-fits-all answer. But here’s a simple guide:
- Choose kyphoplasty if: Your fracture caused visible deformity (hunched back), you’re concerned about cement leakage, or you want the best shot at restoring your height. It’s the safer, more advanced option.
- Choose vertebroplasty if: Your fracture is stable, there’s no major height loss, and you’re looking for the most cost-effective way to stop the pain. It works just as well for pain relief.
Ask your doctor: “Is my fracture causing deformity? What’s the risk of cement leaking? Will this fix my posture?” Don’t just accept the first option they suggest. Both are valid. But they serve different needs.
And remember: these procedures fix the broken bone. They don’t fix osteoporosis. Make sure you’re also working with your doctor on long-term bone health. Otherwise, you’re just putting out fires one at a time.
What happens after the procedure?
After you go home, you’ll be given instructions to avoid heavy lifting and twisting for the first week. Most people return to light work in a few days. Physical therapy might be recommended to rebuild core strength and improve posture.
You’ll need follow-up X-rays in 6 to 12 weeks to check the cement and make sure no new fractures have formed. Your doctor will also check your bone density and adjust your osteoporosis treatment plan.
If you’re still in pain after a month, don’t assume the procedure failed. Sometimes it takes time. But if the pain returns or spreads, tell your doctor right away. New fractures or nerve issues can develop.
Are kyphoplasty and vertebroplasty the same thing?
No. Both use bone cement to stabilize fractured vertebrae, but kyphoplasty adds a balloon step to restore height before injecting cement. Vertebroplasty injects cement directly without trying to lift the bone. Kyphoplasty is more complex and costs more, but reduces cement leakage risk and can improve posture.
Which procedure is better for osteoporosis-related fractures?
Both are effective for pain relief. But kyphoplasty is often preferred for osteoporotic fractures with significant height loss or spinal deformity because it restores more of the original bone shape and has a lower risk of cement leakage. For stable fractures without deformity, vertebroplasty offers similar pain relief at a lower cost.
How soon can I walk after the procedure?
Most patients are encouraged to walk within a few hours after the procedure, once the sedation wears off. You’ll need to avoid heavy lifting and twisting for 24 hours, but light walking and daily activities are usually fine the same day. Full recovery to normal activity takes about 1 to 2 weeks.
Do these procedures cure osteoporosis?
No. Kyphoplasty and vertebroplasty treat the fracture, not the underlying bone weakness. Osteoporosis still needs long-term management with calcium, vitamin D, exercise, and medications like bisphosphonates. Without this, you’re at high risk for future fractures in other vertebrae.
Is kyphoplasty worth the extra cost?
It depends. If your fracture has caused visible spinal deformity or you have very weak bones, the lower risk of complications and better height restoration make kyphoplasty worth the extra $900. If your fracture is stable and pain is your only concern, vertebroplasty offers the same relief at a lower price. Insurance usually covers both if conservative treatments failed first.
How long does the pain relief last?
For most patients, pain relief is long-lasting-often permanent for that specific fracture. The cement stays in place for years. But if you have ongoing osteoporosis, new fractures can occur in nearby vertebrae. That’s not a failure of the procedure; it’s a sign the disease needs better management.







Paul Mason
January 7, 2026 AT 01:39I've seen way too many older folks get vertebroplasty and then wonder why they're still hunched over like a question mark. Kyphoplasty's the move if you care about looking human again. Simple as that.
Katrina Morris
January 8, 2026 AT 06:18I had kyphoplasty last year and wow what a difference. I could breathe again like i'd forgotten how. No more holding my breath when i stand up. Still take my calcium but at least i'm not a crooked stick anymore 😊
LALITA KUDIYA
January 9, 2026 AT 04:49My aunt got vertebroplasty and she's fine now. Pain gone. But she still walks with a hunch. I think if you can afford it kyphoplasty is better for long term. Also less risk of cement leak i heard
Poppy Newman
January 9, 2026 AT 19:09The balloon step sounds like something out of a sci-fi movie 🎈💉 But honestly? If it means I don't look like a question mark for the rest of my life... sign me up. Kyphoplasty all the way.
Christine Joy Chicano
January 9, 2026 AT 20:11The notion that vertebroplasty is ‘just as good’ for pain relief is statistically accurate but clinically reductive. Kyphoplasty doesn’t merely mitigate leakage-it alters biomechanical loading dynamics across adjacent segments. That’s not a luxury; it’s a prophylactic advantage in osteoporotic spines. Ignoring it is like patching a tire but refusing to check the rims.
Anastasia Novak
January 10, 2026 AT 03:56Let me tell you something no one wants to admit: 80% of these procedures are done because insurance won't cover physical therapy or bone meds. They'd rather shove cement into your spine than pay for a damn exercise program. It's a profit-driven band-aid on a systemic failure. 🤡
Jonathan Larson
January 11, 2026 AT 01:29While the technical distinctions between these interventions are well-documented, one must not overlook the broader existential context: human dignity in the face of bodily decay. Restoring verticality is not merely anatomical-it is psychological, social, and spiritual. To stand tall is to reclaim agency.
Elen Pihlap
January 11, 2026 AT 21:39I know someone who got the balloon thing and now she's in more pain because the cement leaked into her spine and now she's got nerve damage and her kids are suing the hospital and I'm just saying maybe we should just stick with painkillers and be done with it
Sai Ganesh
January 12, 2026 AT 04:10In India, many elderly cannot afford kyphoplasty. Vertebroplasty is the only option. Pain relief is real. Height restoration is secondary. We must not romanticize procedures that are inaccessible to most. Practicality over prestige.
Anthony Capunong
January 12, 2026 AT 22:39America's healthcare system is broken. You pay more for kyphoplasty because it's patented by Medtronic. In Canada they just use the cheaper one and it works fine. Stop buying into corporate marketing. It's the same damn cement.
Emma Addison Thomas
January 13, 2026 AT 07:27I think both have their place. My mom had vertebroplasty and she's happy. My neighbor had kyphoplasty and she walks straighter. It's not about which is better-it's about which fits your life. No need to fight over it.
Mina Murray
January 14, 2026 AT 20:12You know what they don't tell you? The balloon is made with nanotech that's secretly linked to CDC tracking chips. They want you to think it's about pain relief but really they're mapping your spine so they can control your movement later. Watch the 2023 Lancet study-read between the lines. They're lying about the mortality drop. It's a cover.