CGM Dose Adjustment Calculator
Calculate Your Adjustment
How It Works
Based on Endocrine Society guidelines, the calculator determines your precise insulin adjustment based on:
- Current glucose level 150 mg/dL
- Trend arrow type Double-up
- Correction factor 1 unit per 50 mg/dL
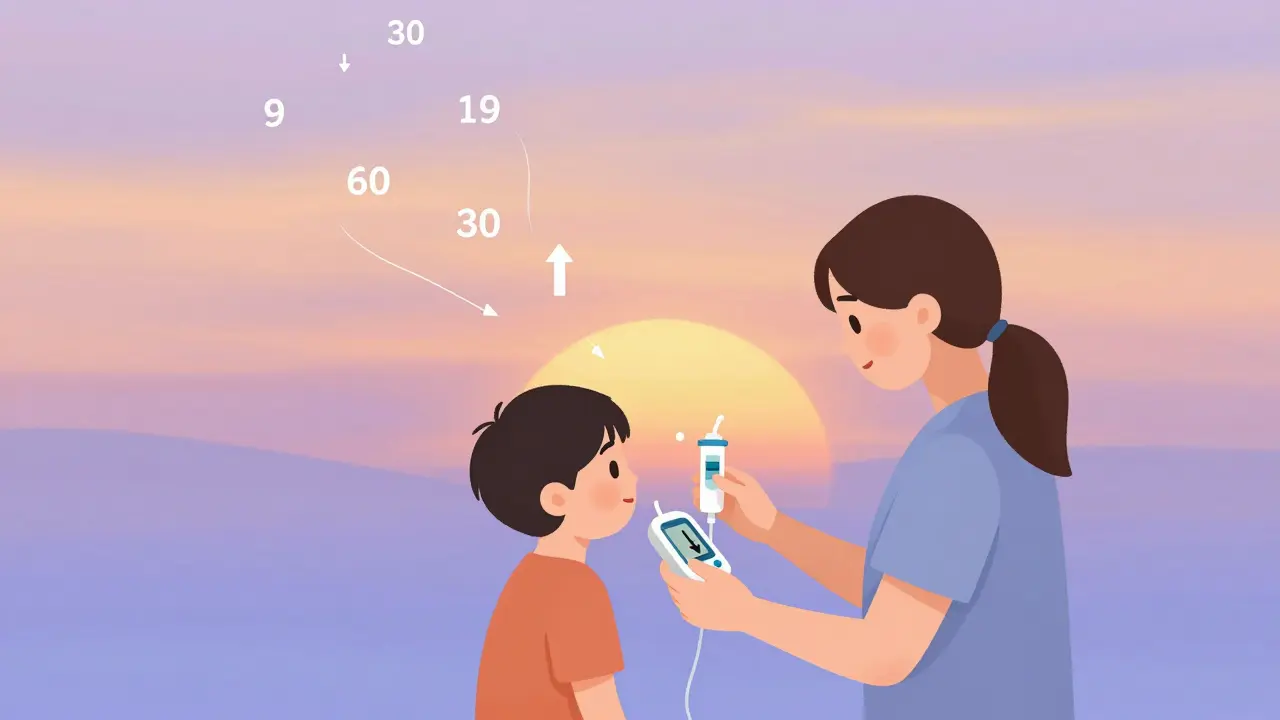
When your glucose is dropping fast and your CGM shows two downward arrows, should you take more insulin? What if your sugar is climbing before breakfast-do you just guess how much to add? For people using insulin or other diabetes medications, CGM trend arrows aren’t just data-they’re life-saving signals. But most people don’t know how to use them right. And that’s dangerous.
What CGM Trend Arrows Actually Mean
Your CGM doesn’t just show your current glucose number. It shows where it’s going. That’s the power. The trend arrows tell you if your blood sugar is rising, falling, or steady-and how fast. Dexcom’s system uses five arrow types: double-up (rising fast), single-up (rising), flat (stable), single-down (falling), and double-down (falling fast). Abbott’s Libre uses similar logic, though the speed thresholds vary slightly. These aren’t guesses. They’re calculated from real-time glucose changes over the last 15 to 30 minutes.Think of it like driving a car. Your glucose number is your speedometer. The trend arrow is your rearview mirror showing if you’re about to hit a wall or hit the gas. If you only look at the speedometer, you’re reacting after the fact. With trend arrows, you can brake before the crash.
Why Traditional Dosing Falls Short
Most people adjust insulin based on their current glucose level and a fixed correction factor-like “1 unit lowers my sugar by 50 mg/dL.” That works fine if your glucose is steady. But it fails when your sugar is moving fast. A 2017 study in Diabetes Technology & Therapeutics found that people using only fingersticks had 28% more low blood sugar events than those using trend arrows. Why? Because a fingerstick at 180 mg/dL could be rising to 250-or falling to 120. You don’t know which. CGM tells you.And here’s the real problem: if your sugar is falling fast and you give a correction dose anyway, you could crash. If it’s rising fast and you don’t act, you’ll spike. That’s why the Endocrine Society published guidelines in 2017-specifically to turn CGM from a monitor into a dosing tool.
The Endocrine Society’s Simple Dose Adjustment Rules
These guidelines removed the guesswork. Instead of saying “increase by 20%,” they gave exact unit changes based on your personal insulin sensitivity. For example, if your correction factor is 1:50 (1 unit lowers glucose by 50 mg/dL), here’s what to do:- Double-up arrow (rising fast): Add 1.2 units to your pre-meal or correction dose
- Single-up arrow (rising): Add 0.8 units
- Flat arrow (stable): No change
- Single-down arrow (falling): Subtract 0.8 units
- Double-down arrow (falling fast): Subtract 1.2 units
For kids, the numbers are smaller: +1.0, +0.6, 0, -0.6, -1.0. These values are based on average insulin action times and have been tested in real patients. You don’t need to calculate percentages. You don’t need a calculator. You just match the arrow to the number.
These adjustments are meant to be added to your normal dose-not replace it. So if you need 4 units for carbs and your sugar is 170 with a double-up arrow, you’d take 4 + 1.2 = 5.2 units. Simple. But only if you know your correction factor. If you don’t, your provider can figure it out by testing how much your sugar drops after 1 unit of insulin during a low-activity time.

When Not to Trust the Arrows
Trend arrows aren’t magic. They can lie. If your sensor just started, if you’re in the middle of a big insulin bolus, or if you’ve just exercised, the reading might be lagging. The guidelines say: don’t adjust if your sensor is less than 2 hours old, if you’ve had signal loss, or if your glucose is below 60 mg/dL and the arrow is double-down-you’re likely in a real low, not just trending that way.Also, don’t adjust if you still have insulin working from a previous dose. That’s called “stacking.” One user on Reddit added 1.2 units for a double-up arrow… but had 2 units of insulin still active from breakfast. Result? A 45 mg/dL low. That’s not the arrow’s fault-it’s the user not checking insulin-on-board (IOB). Always check your pump or app for active insulin before adjusting.
It’s Not Just for Insulin
The 2024 ADA/EASD consensus report expanded this beyond insulin. If you’re on an SGLT2 inhibitor like dapagliflozin or empagliflozin, and your CGM shows glucose under 180 mg/dL but ketones are rising (above 0.6 mmol/L), you might be in euglycemic diabetic ketoacidosis (euDKA). That’s rare but dangerous. In those cases, your provider may tell you to reduce your SGLT2 inhibitor dose or skip it entirely until the ketones drop. CGM helps spot this early because glucose stays normal while ketones build-something a fingerstick would miss.Real People, Real Results
On the TypeOneGrit subreddit, one user cut their weekly lows from 3.2 to 0.7 after using these rules. Another parent said the pediatric tables saved her son’s sleep-she used to wake up every night to check his sugar. Now, she sees a double-down arrow at 2 a.m. and reduces his basal rate by 10% instead of panicking.But it’s not perfect. A 2021 survey of over 1,200 CGM users found 32% didn’t use trend arrows at all. Why? Fear. “I don’t trust myself to do it right,” one said. Another said their doctor never taught them. That’s the biggest barrier-not the tech, but the education.
How to Learn This Right
If you’re new to CGM, don’t wing it. Ask your diabetes educator for a 15-minute session on trend arrows. They should walk you through:- How your personal insulin works (how long it lasts, when it peaks)
- What your correction factor is
- How to read arrows in context (e.g., is this after a meal? After exercise?)
- How to check insulin-on-board
- When to ignore the arrow and go by your usual rules
Dexcom offers printable cheat sheets. The ADA’s 2023 Standards say every insulin user should get this training within 30 days of starting CGM. If your provider hasn’t offered it, ask. It’s not optional anymore-it’s standard care.
What’s Next? AI and Automation
The FDA approved DAFNE+ in 2023-a phone app that auto-calculates your dose based on your CGM trend, carbs, and IOB. In trials, it cut dosing errors by 62%. That’s huge. But even with AI, you still need to understand the basics. You can’t trust a black box if you don’t know why it’s making a suggestion.Verily’s Onduo platform already uses machine learning to predict trends beyond the arrows. In a 2022 study, it cut hypoglycemia by 38%. But those systems are still in early use. For now, the Endocrine Society’s rules are the gold standard-and they’re free, simple, and proven.
Don’t Let Fear Stop You
It’s scary to change how you dose insulin. You might worry you’ll make a mistake. But the real risk is doing nothing. A 2023 JAMA study found only 31% of primary care doctors feel confident teaching this. That means most patients are left to figure it out alone. But you don’t have to be one of them.Start small. Pick one time of day-say, breakfast-and try adjusting your dose based on the arrow. Write down what you did and what your glucose did an hour later. After a few days, you’ll start to see patterns. You’ll learn your body’s rhythm. And you’ll stop guessing.
CGM gave you superpowers. Trend arrows are the trigger. Use them.
Can I use CGM trend arrows if I’m not on insulin?
Yes, but differently. If you’re on SGLT2 inhibitors (like Jardiance or Farxiga), persistent low glucose with rising ketones (euglycemic ketosis) can be dangerous. CGM trend arrows help you spot this early-even when your glucose looks normal. Your provider may advise reducing or pausing your medication if this happens. For other non-insulin drugs like metformin or GLP-1 agonists, trend arrows help you understand how your body responds to food, stress, or activity, so you can adjust meals or timing, not doses.
Do all CGM devices use the same trend arrows?
The symbols are similar, but the speed thresholds vary. Dexcom’s double-up arrow means glucose is rising faster than 2 mg/dL per minute. Abbott’s Libre uses 3 mg/dL per minute for the same symbol. That means the same arrow on two different devices might mean different things. Always check your device’s manual. The Endocrine Society guidelines were based on Dexcom data, but the principles apply to all. If you switch devices, relearn the speed definitions.
What if my CGM says my sugar is falling fast, but I feel fine?
Trust the data, but verify. CGM sensors can lag during rapid changes, especially after exercise or insulin. If you feel fine but the arrow is double-down, check with a fingerstick. If your meter matches, reduce your next insulin dose. If it doesn’t, wait 15 minutes and check again. Don’t treat based on feeling alone-hypoglycemia can sneak up without symptoms, especially if you have hypoglycemia unawareness.
How long does it take to get good at using trend arrows?
Most people get comfortable in 2-4 weeks with daily practice. Start by using arrows only for correction doses, not meals. Keep a log: arrow, dose given, glucose 1 hour later. After 10-15 entries, you’ll start to see how your body responds. The hardest part isn’t the math-it’s overcoming the fear of changing your dose. Once you see your lows drop and your time-in-range improve, it becomes second nature.
Can I use this method with a hybrid closed-loop system?
Yes, but you’re not in control. Hybrid systems like MiniMed 780G or Omnipod 5 use trend arrows to auto-adjust basal insulin. But they don’t adjust boluses for meals unless you tell them. So you still need to know how to use arrows for mealtime doses. The system handles the background insulin; you handle the food. Understanding trend arrows helps you know when the system is working well-or when you need to step in.







Alexandra Enns
January 23, 2026 AT 21:08Wow, so you're telling me we're supposed to trust a device that can't even tell if I'm on the toilet or having a sugar crash? My Dexcom once told me I was dropping fast while I was literally eating a donut. This isn't medicine, it's sci-fi fanfiction with extra steps. I'd rather guess than let a plastic sensor dictate my life.
Marie-Pier D.
January 23, 2026 AT 22:09Thank you for writing this!! 🙏 I used to panic every time I saw a double-down arrow-now I just subtract 0.8 units like you said and breathe. My son’s bedtime sugars went from chaotic to calm in two weeks. You’re right-it’s not magic, it’s math. And math doesn’t judge. 💙
Izzy Hadala
January 23, 2026 AT 23:05While the proposed dose adjustments based on CGM trend arrows are conceptually sound, the clinical validity of these specific unit increments (e.g., ±0.8 or ±1.2) requires further validation across heterogeneous populations. The referenced 2017 study demonstrated reduced hypoglycemia, but did not isolate the contribution of trend arrows versus continuous monitoring per se. A randomized controlled trial with stratified insulin sensitivity cohorts is warranted before universal adoption.
Elizabeth Cannon
January 24, 2026 AT 08:29OMG YES this is life changing. I used to dose like a robot-'1 unit per 50' no matter what. Then I started using the arrows and my highs dropped and my lows? Gone. Like, poof. No more 3am alarms. My endo didn’t even mention this stuff. Why? 😭
Shelby Marcel
January 26, 2026 AT 05:33wait so if my sugar is 180 and double up i add 1.2? but what if i just ate? i thought you were supposed to wait? im confused
Luke Davidson
January 27, 2026 AT 06:38Y’all. I used to think CGM arrows were just fancy decoration. Like, ‘oh look, a little arrow! Cute.’ Then I got lazy and stopped checking my fingersticks. One Tuesday, I saw a double-down at 82 and thought ‘eh, I feel fine.’ Four hours later, I was in the ER with a glucose of 38. That was the day I started listening. Now I treat the arrow like my third eye. Don’t wait until you’re unconscious to learn this stuff. Your future self will thank you.
Karen Conlin
January 28, 2026 AT 23:09THIS. This right here is the missing link in diabetes care. We’ve been teaching people to react to numbers instead of predicting movement. It’s like driving blindfolded and hoping you don’t hit a tree. The Endocrine Society guidelines? Free. Simple. Proven. If your provider hasn’t taught you this, ask for a referral to a CDE. Seriously. It’s not extra-it’s essential. You deserve to live without fear.
Sushrita Chakraborty
January 29, 2026 AT 05:44It is imperative to note that the application of these guidelines must be individualized, as insulin sensitivity varies significantly among individuals based on factors such as age, body mass index, physical activity levels, and comorbid conditions. Moreover, the temporal dynamics of glucose absorption and insulin pharmacokinetics necessitate a comprehensive understanding of insulin-on-board before any adjustment is undertaken. Misapplication may lead to iatrogenic hypoglycemia.
Sawyer Vitela
January 30, 2026 AT 06:321.2 units? That’s a random number pulled from a hat. No clinical trial ever tested that exact increment. You’re just giving people permission to guess louder.
Shanta Blank
January 30, 2026 AT 21:18So let me get this straight-you’re telling me to trust a $1000 sensor that sometimes thinks I’m crashing while I’m eating pizza… and now I’m supposed to inject MORE insulin if it says I’m rising? What if it’s wrong? What if I die? What if my kid dies? This isn’t advice, it’s a death wish wrapped in a Dexcom sticker.
Vatsal Patel
January 31, 2026 AT 20:08How quaint. You treat glucose like a chessboard, moving pieces with arithmetic. But the body is not a machine-it is a symphony of chaos, hormones whispering in ancient tongues. The arrow is not truth-it is a shadow cast by the flame of metabolism. You think you control it? You are merely a guest at the table. The real power lies not in the number, but in the silence between heartbeats. And yet… you still take the insulin, don’t you? Of course you do. Because fear is the only thing that never lies.