Anticholinergic Burden Calculator
Add Your Medications
Your Current Burden
Medication List
Many older adults take antihistamines every day-not for allergies, but for sleep. A nightly dose of Benadryl seems harmless. It’s over-the-counter, cheap, and widely recommended by well-meaning friends or even pharmacists. But what if that little pill, taken for years, is quietly adding up with other medications to damage memory, increase falls, and raise the risk of dementia? This isn’t speculation. It’s measurable, documented, and preventable.
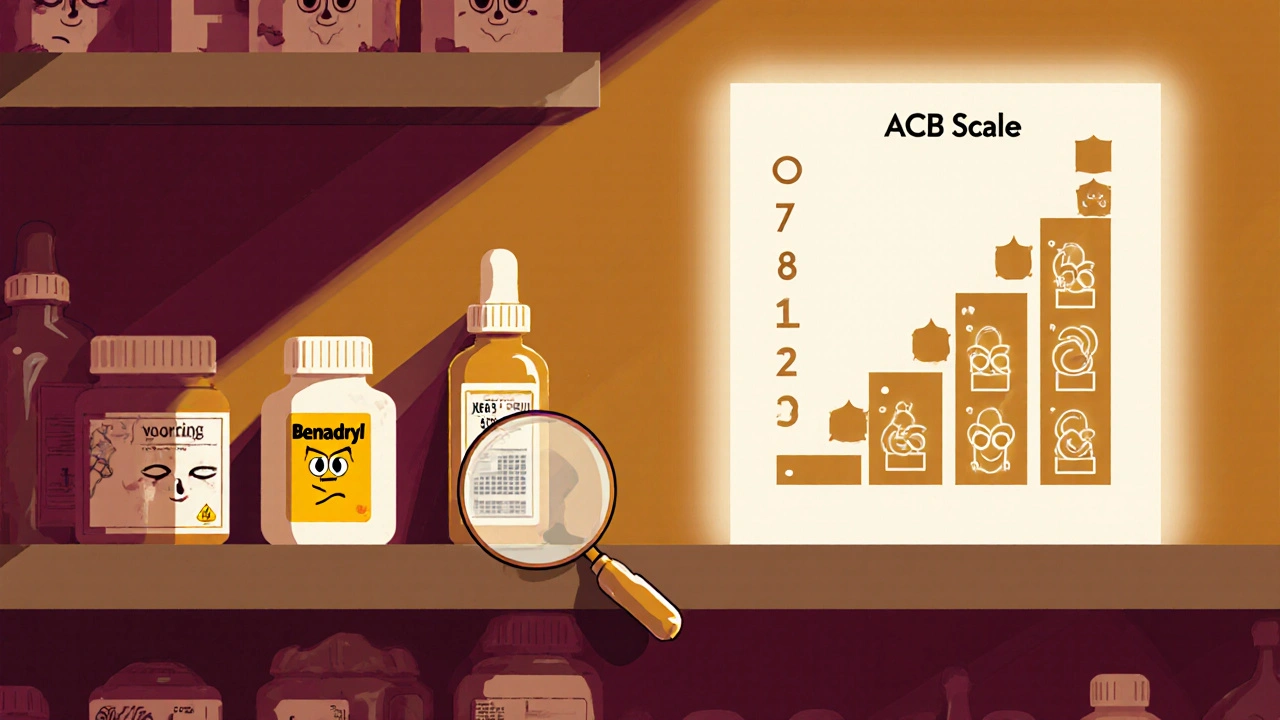
What Is Cumulative Anticholinergic Burden?
Anticholinergic burden isn’t about one drug. It’s about the total effect of all the drugs you take that block acetylcholine, a key brain chemical. This chemical helps with memory, attention, muscle control, and even bladder function. When too many medications interfere with it, your body starts to pay the price. The most widely used tool to measure this is the Anticholinergic Burden (ACB) Scale. It rates every medication on a scale from 0 to 3:- Score 0: No anticholinergic effect
- Score 1: Mild effect
- Score 2 or 3: Strong effect
Why Antihistamines Are a Silent Culprit
Not all antihistamines are the same. Second-generation ones like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have little to no anticholinergic effect. They’re designed to stay out of the brain. But first-generation antihistamines? They’re built to cross the blood-brain barrier. That’s why they make you sleepy. And that’s exactly why they’re dangerous over time.- Diphenhydramine (Benadryl): ACB score of 3
- Chlorpheniramine (Chlor-Trimeton): ACB score of 3
- Hydroxyzine (Atarax): ACB score of 2
What Other Medications Make It Worse?
The real danger isn’t just antihistamines alone. It’s what they’re taken with. Here’s what often stacks up with those nightly Benadryls:- Tricyclic antidepressants like amitriptyline (ACB score 3)
- Bladder medications like oxybutynin (ACB score 3)
- Parkinson’s drugs like benztropine (ACB score 3)
- Antipsychotics like olanzapine (ACB score 2)
- Some pain meds like cyclobenzaprine (ACB score 2)
Real People, Real Consequences
On Reddit’s r/geriatrics, a caregiver wrote: “My 78-year-old mom was diagnosed with early dementia. She forgot names, got lost in her own house. We stopped her nightly Benadryl and her amitriptyline. Within six weeks, she remembered her grandchildren’s birthdays again.” That’s not an isolated story. Hospitals across the U.S. and Australia are seeing this pattern. A 72-year-old patient in a NPS MedicineWise case study had an ACB score of 5 from diphenhydramine, oxybutynin, and amitriptyline. After switching to non-anticholinergic alternatives, his falls dropped by 75% and his mental clarity improved dramatically. Side effects aren’t always dramatic. Dry mouth? Blurred vision? Constipation? These are often dismissed as “just aging.” But they’re signs your body is drowning in anticholinergic effects.How to Check Your Burden
You don’t need a doctor’s order to start checking. Here’s how:- Write down every pill, patch, or liquid you take daily-even vitamins and OTC meds.
- Look up each one on the ACB Scale database (or ask your pharmacist).
- Add up the scores.
- If the total is 3 or more, talk to your doctor about alternatives.
What Are the Safer Alternatives?
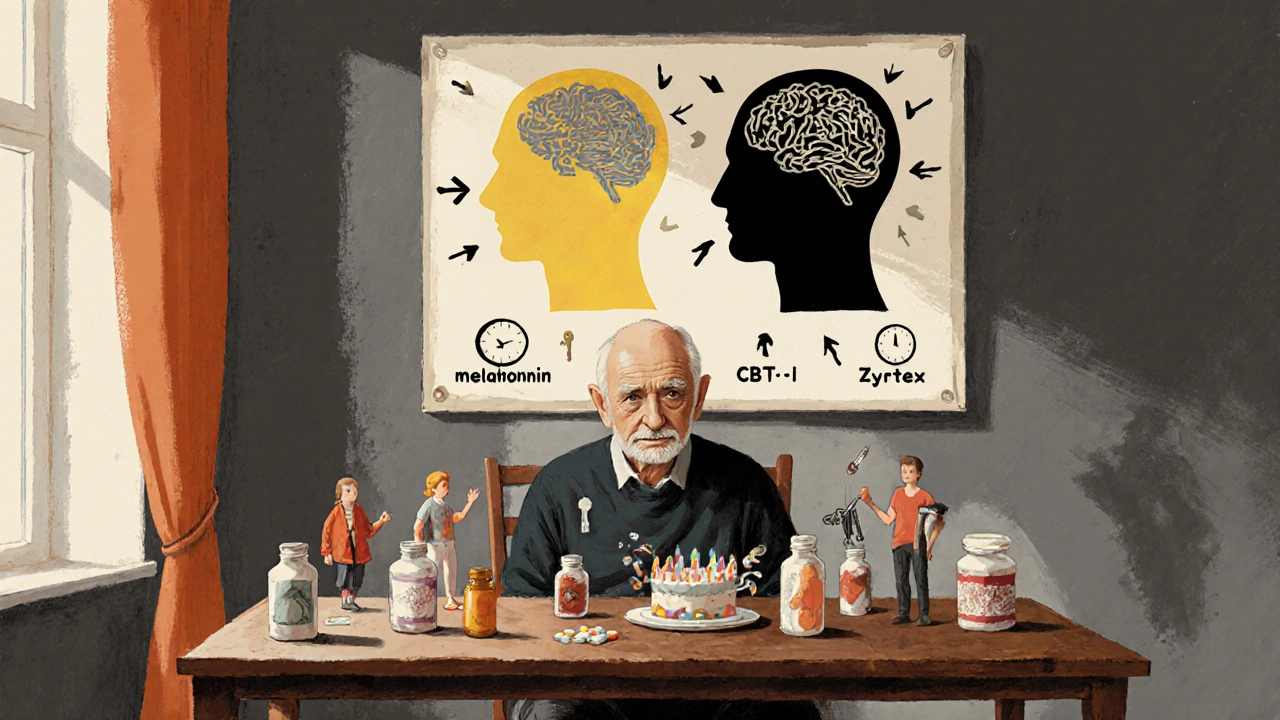
For allergies, switch to second-generation antihistamines:- Switch from diphenhydramine → cetirizine (Zyrtec)
- Switch from chlorpheniramine → loratadine (Claritin)
- Melatonin (0.5-3 mg, 30 minutes before bed)
- Cognitive behavioral therapy for insomnia (CBT-I)
- Improved sleep hygiene-dark room, no screens, consistent bedtime
Why Doctors Miss This
It’s not that doctors don’t care. It’s that they’re overwhelmed. Most don’t have time to review every OTC med a patient takes. And many patients don’t even think to mention their nightly Benadryl. Plus, 70% of strong anticholinergics are sold over the counter. No prescription means no flag in the system. No warning label says, “This may cause dementia if taken daily for years.” The FDA added a warning to Benadryl labels in 2017-but it’s buried in small print. Most people never see it.What’s Changing Now?
The tide is turning. The American Geriatrics Society updated its Beers Criteria in 2023 to say: “Chronic use of first-generation antihistamines should be avoided in older adults due to strong evidence of cognitive impairment-even at low doses.” Hospitals in Australia and the U.S. are now embedding ACB checks into electronic health records. If a doctor prescribes oxybutynin to someone already on diphenhydramine, the system flags it. Preliminary results show a 47% drop in inappropriate prescribing. Medicare plans are starting to tie quality ratings to reduced anticholinergic burden. That means hospitals and pharmacies now have a financial reason to care.What You Can Do Today
This isn’t about fear. It’s about awareness.- Check your own meds. Don’t assume OTC means safe.
- Ask your pharmacist to run an anticholinergic burden check.
- Bring your pill bottle to your next doctor visit-not just the list.
- If you’re taking more than one anticholinergic, ask: “Can any of these be stopped or switched?”
Can antihistamines cause dementia?
Long-term use of first-generation antihistamines like diphenhydramine and chlorpheniramine is linked to a higher risk of dementia, especially when combined with other anticholinergic medications. A 2015 JAMA study found that people who took strong anticholinergics for more than three years had a 54% increased risk of dementia. Antihistamines made up nearly 30% of the strong anticholinergic drugs in that study.
Is Benadryl safe for seniors to use occasionally?
Occasional use-for example, once a week for an allergic reaction-is unlikely to cause harm. But nightly use for sleep, even for a few months, adds up. The risk isn’t from one dose. It’s from daily exposure over months or years. The American Geriatrics Society recommends avoiding first-generation antihistamines entirely in older adults because of the cumulative effect.
What are the signs of too much anticholinergic burden?
Common signs include confusion, memory lapses, trouble concentrating, dry mouth, blurred vision, constipation, urinary retention, dizziness, and unexplained falls. These are often mistaken for normal aging-but they can reverse once the medications are adjusted. If you or a loved one has these symptoms and takes multiple medications, ask about anticholinergic burden.
Are second-generation antihistamines like Zyrtec or Claritin safe?
Yes. Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) have little to no anticholinergic effect because they don’t cross into the brain. They’re the preferred choice for allergies in older adults. Their ACB score is 0 or 1, compared to 3 for Benadryl.
Can I stop taking my anticholinergic meds on my own?
No. Stopping some medications suddenly can be dangerous-especially antidepressants or bladder drugs. Always talk to your doctor or pharmacist first. They can help you taper safely and replace the medication with a safer alternative. Many people successfully switch without losing symptom control.
How do I find out my anticholinergic burden score?
Ask your pharmacist or doctor to use the Anticholinergic Burden (ACB) Scale. You can also check the online ACB database by searching your medication names. Write down every pill you take-including over-the-counter and herbal products. Then add up the scores. A total of 3 or higher means you’re at increased risk and should review your regimen.



april kakoske
October 29, 2025 AT 09:11i used to take benadryl every night for years 😅 never thought it was doing anything but helping me sleep. now i feel like a fool. just checked my meds-turns out i had acb score of 4. switched to melatonin and my brain feels lighter. no more brain fog at 3pm.
Pradeep Meena
October 30, 2025 AT 05:29this is american bullshit. in india we take antihistamines since childhood and no one gets dementia. your doctors are just selling expensive pills. stop scaring old people with science nonsense.
Rishabh Jaiswal
October 30, 2025 AT 21:17lol u guys r so worried about acb score but u dont even know what acetylcholine is. its a neurotransmitter u dumbass. benadryl is fine if u dont take it with other shit. i took it for 15 years and im 68 and still run marathons. stop listening to medias.
May Zone skelah
October 31, 2025 AT 14:02Let me just say, as someone who has spent years studying the phenomenology of pharmacological alienation in geriatric populations, this post is not merely informative-it is a *cultural reckoning*. The anticholinergic burden isn’t just a medical metric; it’s a metaphor for our society’s pathological relationship with convenience, with sedation, with the quiet erasure of self through chemical compliance. We’ve outsourced our sleep to a pill, our anxiety to a prescription, our dignity to a label that reads 'OTC'-as if safety were a commodity you could buy at CVS. And now? Now we’re waking up to the fact that the ghost in the machine was never the dementia-it was the *negligence*.
Dale Yu
October 31, 2025 AT 14:59you people are so weak. if you cant handle a little drowsiness you dont deserve to live. benadryl is cheaper than therapy and it works. stop crying about dementia. everyone dies anyway. just take the pill and shut up.
Kshitij Nim
November 1, 2025 AT 06:37good post. i work with seniors daily. seen this pattern a hundred times. mom on benadryl + oxybutynin + amitriptyline. confused all the time. family blames aging. we switch her to mirabegron + sertraline + melatonin. she starts remembering names again. no magic. just science. ask your pharmacist. its free.
Scott Horvath
November 1, 2025 AT 21:45i had no idea my nightly zzzquil was basically a brain fog bomb. just looked up my meds-turns out i was on a 5. wow. made an appt with my pharmacist today. she laughed and said 'oh honey youre not alone'. we swapped my diphenhydramine for cetirizine and now i sleep better without the next-day zombie mode. small change. big difference.
Armando Rodriguez
November 2, 2025 AT 03:42This is an exceptionally well-researched and urgently needed public health message. The cumulative anticholinergic burden is one of the most underrecognized iatrogenic risks in geriatric medicine. I have personally reviewed over 200 medication regimens in the past year alone, and nearly 60% of patients over 65 were on at least one high-risk anticholinergic without clinical justification. The data is unequivocal. The solution is simple: pharmacist-led medication reconciliation. Every senior deserves a full med review at least annually. I encourage all clinicians to implement this as standard of care.
jennifer sizemore
November 3, 2025 AT 16:32my grandma stopped her benadryl after reading this and now she tells stories from when she was 12 again. it was like flipping a switch. i cried. thank you for writing this. i shared it with my whole family. we’re all checking our meds now. no shame in asking. your brain matters more than you think.
matt tricarico
November 4, 2025 AT 15:27This is peak performative medicine. The ACB scale is a statistical artifact with no clinical validity in isolation. You're replacing one placebo with another-melatonin? CBT-I? Please. The real issue is the pharmaceutical industry's fearmongering to push expensive alternatives. Benadryl has been used safely for 70 years. If you're worried about dementia, stop scrolling Reddit and go for a walk.