If you’re taking insulin, biologics, or certain vaccines, your medicine isn’t just sitting on the shelf-it’s fighting to stay alive. Even a few hours in a hot car or a freezer drawer can turn your life-saving drug into a useless, even dangerous, substance. And most people have no idea how fragile these medications really are.
Why Some Medications Need the Fridge
Not all pills and liquids are created equal. While your blood pressure medicine or antibiotics can handle your bathroom cabinet, a growing number of drugs-mostly biologics, insulin, and vaccines-need to stay between 2°C and 8°C (36°F to 46°F). That’s the sweet spot. Too cold, and the proteins freeze and break apart. Too warm, and they start to degrade-fast.Insulin is the most common example. If you leave a vial in a hot car at 35°C for 24 hours, it can lose up to 40% of its strength. That’s not a small drop-it’s enough to send your blood sugar into dangerous territory. Vaccines like MMR or flu shots? They’re even more sensitive. At room temperature, some lose effectiveness in just days. And biologics like Remicade® or Humira®? They’re made from living cells. Mess with their temperature, and you risk a treatment failure-or worse.
The FDA and World Health Organization agree: this 2°C to 8°C range isn’t a suggestion. It’s a requirement. And it’s not just about potency. Improper storage has been linked to hospitalizations. In 2021, a patient developed diabetic ketoacidosis after using insulin that had been left unrefrigerated for over a week. That’s not rare. It’s preventable.
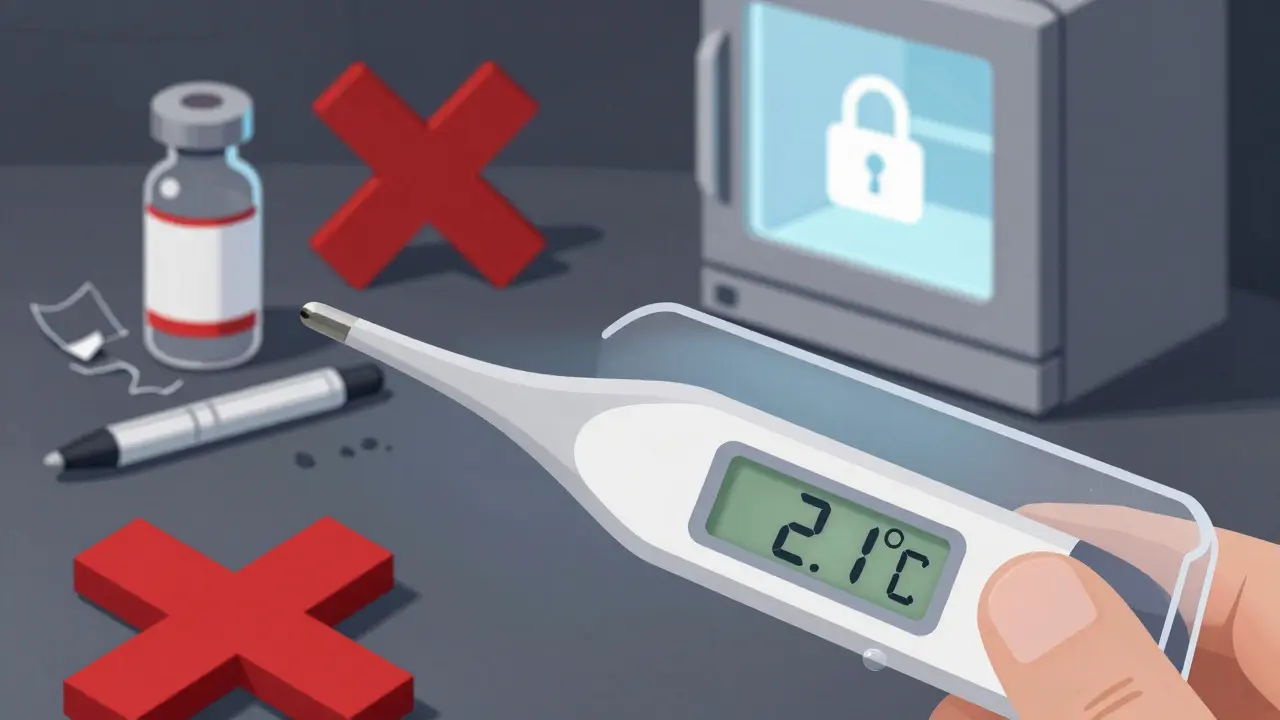
Where Not to Put Your Medication
Your kitchen fridge might seem like the obvious choice-but it’s a minefield. The door shelves? They’re the warmest part, often hitting 11°C. The back? That’s where it’s coldest, sometimes dipping below freezing. And if you’ve ever opened the fridge 20 times a day? You’re creating temperature swings that your meds can’t handle.Don’t store insulin in the vegetable crisper. Don’t tuck vaccines behind the milk carton. Don’t leave your biologic pen on the counter while you make coffee. These aren’t just bad ideas-they’re risks.
Even your freezer is off-limits. Freezing insulin, even briefly, destroys its structure. Thawing it won’t fix it. Once frozen, it’s trash. No exceptions. I’ve seen patients try to save frozen insulin by letting it sit out. It doesn’t work. And when it fails, the consequences are real.
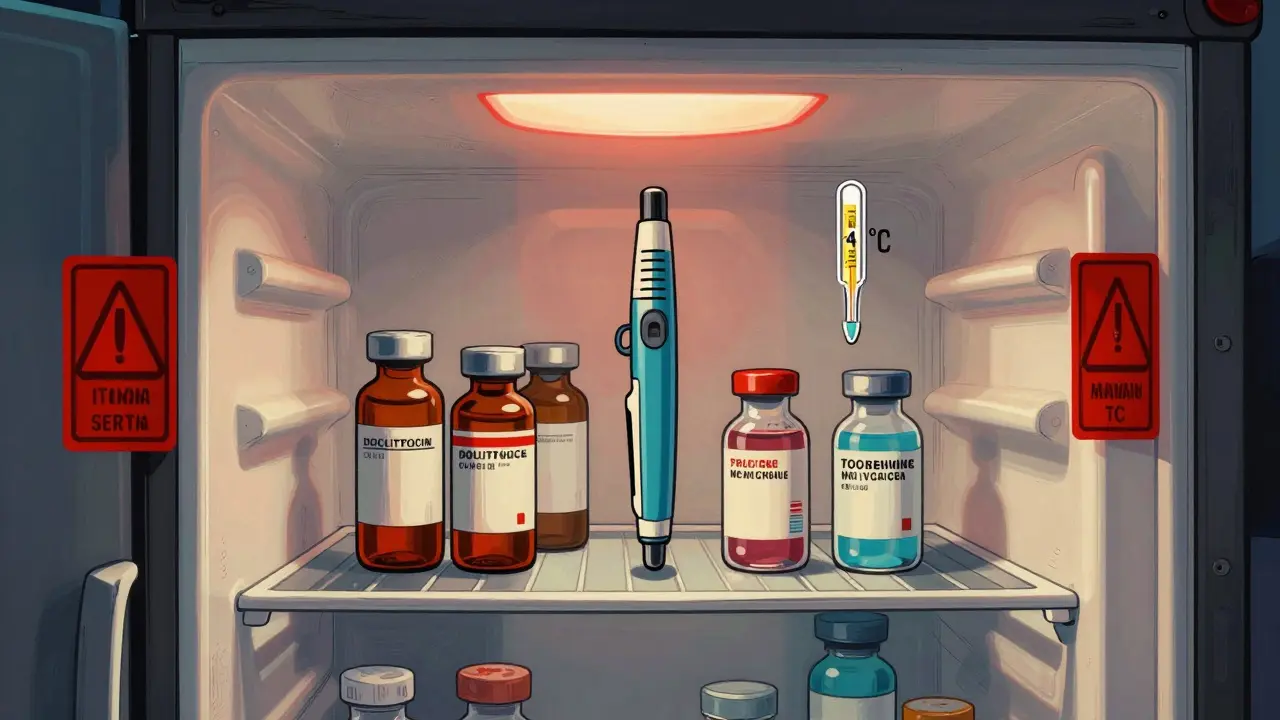
Where to Store It-The Right Way
The best spot in your fridge is the middle shelf, away from the door and the back wall. That’s where temperatures are most stable. Use a small, dedicated container-a plastic box with a lid-to keep your meds organized and protected from moisture and spills.But here’s the truth: most household fridges aren’t built for medicine. A 2022 study found that even in a well-maintained fridge, temperatures can swing between 1.5°C and 10.2°C. That’s a 8.7°C range. For insulin? That’s a problem.
That’s why many people-especially those on daily biologics-use a dedicated medication refrigerator. These aren’t fancy gadgets. Basic models like the Whynter FM-50G cost under $200. They’re small, quiet, and maintain a steady 4°C. No more guessing. No more risks.
And don’t forget a digital thermometer. You can buy one for under $30 that logs min/max temps. Check it once a week. If it’s ever above 8°C or below 2°C, your meds might be compromised. Replace them. Don’t risk it.

What Happens When Things Go Wrong
Let’s say you left your insulin in a car on a 30°C day for three hours. You didn’t notice. You used it the next morning. Your blood sugar spikes. You think it’s your diet. Your pump. Your stress. But it’s the medicine.That’s the silent danger. Degraded meds don’t scream. They just stop working. You don’t feel it until it’s too late.
A 2023 GoodRx survey of over 1,200 insulin users found that 68% had experienced unexplained blood sugar swings they later traced to temperature issues. Over half said they didn’t even know their meds needed refrigeration-until something went wrong.
And it’s not just insulin. Patients on injectable biologics for rheumatoid arthritis or Crohn’s disease report flare-ups after switching to a new bottle-only to find the previous one had been left on the counter for weeks. The new bottle works. The old one didn’t. The difference? Temperature.
Traveling With Refrigerated Medications
Traveling is where most people fail. A 48-hour flight. A road trip. A weekend away. Your fridge stays home. What do you do?Use a validated insulated cooler. Brands like TempAid MediCool or MedKits keep meds between 2°C and 8°C for up to 48 hours. Add a reusable ice pack designed for pharmaceuticals-not regular ice. Water can leak. Gel packs can melt. These are made to stay dry and cool.
For short trips under 24 hours, some newer insulins (like Novo Nordisk’s newer formulations) can handle up to 37°C for a week. But don’t assume yours can. Always check the label. If it says “refrigerate,” assume it needs it-even if you’ve heard otherwise.
And never check your meds in luggage. Checked bags can freeze in cargo holds or bake in hot terminals. Always carry them with you. Keep them in your carry-on, in a small cooler, next to your passport.
What’s Changing-and What to Watch For
The rules are shifting. Manufacturers are starting to test stability under warmer conditions. Novo Nordisk now says some newer insulins can stay at 37°C for up to 7 days. That’s a big deal. But it’s not universal. Not all insulins. Not all biologics.That’s why you can’t rely on hearsay. Your friend’s insulin lasts a month on the counter? That’s not your insulin. That’s not your drug. Always read the manufacturer’s instructions. They’re printed for a reason.
Smart fridges are coming too. Samsung’s 2023 Family Hub model includes a medication storage mode that locks the temperature to 3°C-5°C. It’s not cheap, but for someone on daily biologics, it’s a game-changer.
And the trend is clear. By 2030, the American Society of Health-System Pharmacists predicts that 30% of all prescriptions will need refrigeration. That’s up from 15% today. If you’re on chronic treatment, this isn’t a one-time issue. It’s a lifelong responsibility.
What to Do Right Now
If you’re taking a refrigerated medication, here’s your action list:- Find the label. Read the storage instructions. If it says “refrigerate,” do it-even if you think it’s unnecessary.
- Check your fridge. Use a digital thermometer. Is the middle shelf between 2°C and 8°C? If not, adjust or move your meds.
- Get a dedicated container. Keep your meds in a small box, away from raw meat and strong smells.
- Never freeze. Ever. If it freezes, throw it out.
- When traveling, use a validated cooler. Don’t guess.
- Replace meds if you suspect temperature exposure. Better safe than sorry.
There’s no magic trick. No shortcut. Just consistency. Your life depends on it.
Can I store insulin at room temperature after opening it?
Yes, most insulin vials and pens can be kept at room temperature (up to 30°C) for 28 to 30 days after first use. But only after they’ve been properly refrigerated until opened. Once you take it out of the fridge, write the date on the label. After 28 days, throw it away-even if it still looks clear. Never reuse insulin past its expiration date, even if it’s been refrigerated.
What if my medication freezes accidentally?
If your insulin, vaccine, or biologic freezes-even once-do not use it. Freezing permanently damages the protein structure. Thawing won’t fix it. You might not see a difference in color or texture, but the potency is gone. Dispose of it safely and get a new one. Never risk using frozen medication.
Do all vaccines need refrigeration?
Most do. Vaccines like MMR, flu shots, shingles, and COVID-19 mRNA vaccines require 2°C to 8°C storage. Some, like the live varicella vaccine, need even colder storage-between -50°C and -15°C. Always check the manufacturer’s label. If it says “refrigerate,” assume it means 2°C to 8°C. Never store vaccines in the door of your fridge. Always keep them on the middle shelf.
Can I use a regular cooler instead of a pharmaceutical one?
For short trips (under 24 hours), a regular insulated cooler with ice packs can work-but it’s risky. Regular ice melts and can leak. Ice packs can get too cold and freeze your meds. Use only coolers designed for medications, like TempAid or MedKits. They use phase-change materials that stay in the 2°C-8°C range. If you don’t have one, ask your pharmacist-they often lend them out.
What should I do during a power outage?
Keep your fridge closed. A full fridge can stay cold for up to 24 hours. If the outage lasts longer, move your meds to a cooler with ice packs. If you’re unsure how long your meds were exposed to unsafe temperatures, contact your pharmacist or doctor. When in doubt, replace them. It’s cheaper than a hospital visit.






jesse chen
December 26, 2025 AT 22:12I had no idea insulin could lose 40% of its potency in just a hot car. I’ve been keeping mine on the counter because it’s ‘easier’-but now I’m moving it to the middle shelf. Thanks for the wake-up call.
Also, I just bought a $25 digital thermometer for my fridge. Best $30 I’ve ever spent.
And yes-I’m using a plastic box now. No more mixing with leftover chicken.
So many people don’t realize this isn’t about convenience. It’s about survival.
Joanne Smith
December 27, 2025 AT 06:58Oh honey, you didn’t just write an article-you wrote a survival guide for people who treat their meds like a forgotten avocado.
‘Don’t store vaccines behind the milk carton’-as if we’re all trying to win a game of ‘How Many Ways Can I Ruin My Biologic Today?’
I’ve got a little fridge in my closet labeled ‘LIFE SUPPORT’ and I guard it like it’s the last slice of pizza at a party. You’re welcome, future me.
Prasanthi Kontemukkala
December 29, 2025 AT 01:27As someone from India where power cuts are normal and fridges are often shared in households, this post is a lifeline.
Many of us don’t have the luxury of a dedicated medication fridge, but we can still be smart-use a thermos with ice packs, keep meds in a cool corner away from sunlight, and check temperatures when you can.
It’s not perfect, but it’s better than nothing. Thank you for reminding us that even small steps matter.
And yes-never freeze. I learned that the hard way with my mom’s insulin. She was lucky she didn’t end up in the hospital.
Angela Spagnolo
December 29, 2025 AT 20:02so i just realized i’ve been storing my humira pen in the fridge door for like 8 months???
oh my god
and i thought my blood sugar was just being dramatic
why did no one tell me this
i’m getting a thermometer today
and a little box
and possibly crying
thank you for this
so much
really
Sarah Holmes
December 30, 2025 AT 15:00Let’s be honest: this isn’t about medication. It’s about systemic neglect. Why should a diabetic person have to spend $200 on a mini-fridge just to stay alive? Why isn’t this covered by insurance? Why is the burden placed on the sick to become temperature engineers? This is healthcare capitalism at its most grotesque.
And don’t get me started on how pharma companies market these drugs as ‘convenient’ while knowing full well they’re fragile. Hypocritical. Exploitative. Unforgivable.
Kuldipsinh Rathod
January 1, 2026 AT 01:42Bro, I used to keep my insulin on the kitchen counter like it was a soda can. Now I have a tiny cooler in my bag for work. No more guessing. No more panic. Just chill. Literally.
SHAKTI BHARDWAJ
January 2, 2026 AT 01:39you say don’t freeze it but what if you do? like what if you’re poor and you just have one vial and your fridge breaks and you thaw it and use it anyway? you think they care? hospitals don’t care. insurance doesn’t care. you just die quietly and they move on to the next person.
so yeah. don’t freeze it. but also? the system is rigged.
and you’re lucky if you even have a fridge.
Matthew Ingersoll
January 3, 2026 AT 10:25My grandmother in rural Nebraska used to store her insulin in a bucket of well water during summer power outages. She never had a problem. She lived to 94.
Maybe the science is new. Maybe the rules are changing. But people have survived this long without a $200 fridge. Don’t let perfection become the enemy of practicality.
carissa projo
January 4, 2026 AT 21:31I used to think this was overkill-until I saw my best friend’s blood sugar spike for three weeks and no one could figure out why.
Turns out her biologic had been sitting on the counter for weeks because she thought ‘it’s opened now, so room temp is fine.’
She didn’t know it needed refrigeration even after opening.
She cried when she found out. I cried with her.
We’re not just managing a disease-we’re managing a fragile, invisible system that no one teaches you about.
This post? It’s not just informative. It’s a quiet act of love.
Thank you for writing it.
And if you’re reading this and you’re on a refrigerated med? Please. Check your fridge today. It might save your life.
josue robert figueroa salazar
January 6, 2026 AT 14:12I left mine in the car. It didn’t work. I got hospitalized. Now I carry a cooler. Don’t be me.