Side Effect Onset Calculator
Track When Side Effects Might Appear
Enter your medication start date and select the drug class to see typical side effect onset windows based on clinical research.
Your Expected Onset Window
Note: This tool shows typical patterns based on clinical studies. Individual reactions may vary. Always consult your doctor.
Ever started a new medication and wondered if that weird headache, muscle ache, or swollen lip was just bad luck-or actually caused by the drug? You’re not alone. Many people assume side effects show up right away, but that’s not always true. Some hit within hours. Others creep in weeks or even months later. Knowing when side effects typically appear can save you from misdiagnosis, unnecessary tests, or even stopping a drug that’s actually helping you.
Why Timing Matters More Than You Think
It’s not enough to know what side effects a drug can cause. You need to know when they’re likely to show up. That’s called time-to-onset (TTO). This isn’t just academic-it’s clinical gold. If you develop fatigue two weeks after starting a new pill, and your doctor assumes it’s stress or aging, you might never get the right answer. But if they know that pregabalin commonly causes dizziness within the first week, they’ll connect the dots faster. The science behind this isn’t new. Since the 1990s, researchers have been mapping how different drugs trigger reactions over time. Today, we use advanced models like the Weibull distribution to predict these patterns. The shape of that curve tells you everything: Is the risk highest right away? Does it build slowly? Or stay steady? Most reactions-about 78%-happen early. But that doesn’t mean the others don’t matter.Fast-Onset Reactions: Hours to Days
Some side effects are like a lightning strike. They show up fast because the drug interacts directly with your body’s chemistry. Take ACE inhibitors like lisinopril or enalapril. One known side effect is angioedema-swelling of the face, lips, or throat. For some people, it happens within hours, especially if it’s triggered by histamine. But here’s the twist: for others, it can show up as late as six months in. That’s why doctors miss it. If you got swelling at month four and didn’t tell your doctor you were on an ACE inhibitor, they’ll blame allergies, stress, or even a bug. Then there’s ciprofloxacin, a common antibiotic. The median time for peripheral neuropathy (nerve pain, tingling, burning) is exactly two days. Studies show women experience this even faster than men-two days versus four. If you’re on this drug and your foot starts tingling on day three, don’t wait. Call your doctor. This isn’t normal muscle soreness. It’s a known, time-specific reaction. Even acetaminophen (Tylenol) can cause liver damage-but not after months. It hits fast. Within 24 hours if you overdose. That’s why you’re told not to take more than 4,000 mg a day. It’s not about long-term use. It’s about a single massive dose overwhelming your liver’s ability to detoxify.Mid-Term Reactions: Days to Weeks
This is where most people get confused. Symptoms appear after a few days or weeks, and they assume it’s something else. Statins like atorvastatin or simvastatin are classic examples. Many patients blame muscle pain on the drug. But here’s the surprise: a major 2021 study found that statin users and placebo users reported muscle pain at almost identical rates. When patients stopped taking either the real drug or a sugar pill, over half felt better within three days. That’s not the drug. That’s the nocebo effect-your brain expecting side effects so hard it creates them. Still, some people do have true statin intolerance. For them, muscle pain often starts between one and four weeks. That’s the window to watch. If pain hits day 10 and gets worse, talk to your doctor. Don’t assume it’s just aging. Don’t assume it’s all in your head. Just track it. Pregabalin and gabapentin (used for nerve pain and seizures) have a median onset of 19 and 31 days, respectively. But patient reviews show that over half report dizziness or fatigue within the first week. Why the mismatch? Because people don’t always wait for the median. They notice symptoms early and report them. The median is just the middle point-half experience it sooner, half later.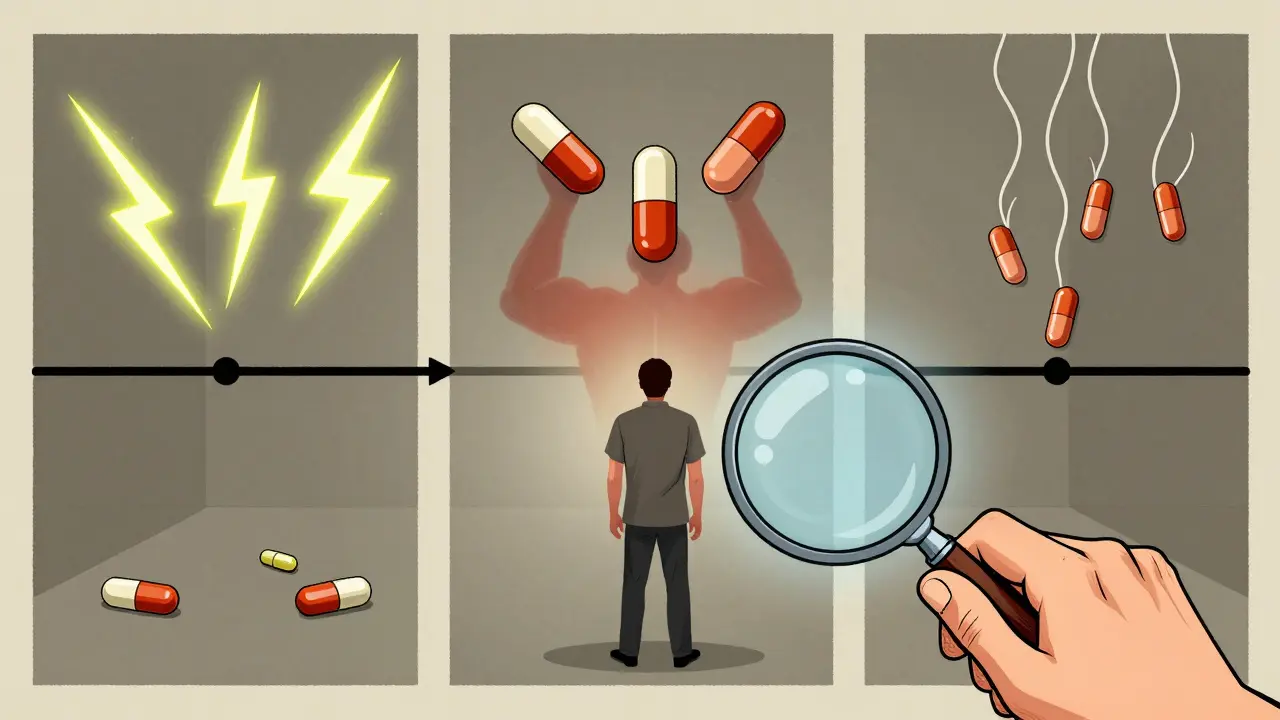
Delayed Reactions: Weeks to Months
These are the sneaky ones. They make you doubt yourself. They make doctors doubt you. Interferon beta-1a, used for multiple sclerosis, has one of the longest known time-to-onset patterns for nerve pain: 526.5 days-almost 18 months. That’s longer than most people stick with the drug. If you develop tingling in your hands after a year and a half, you might never link it to the medication. Natalizumab, another MS drug, causes peripheral neuropathy with a median onset of 141.5 days-about four and a half months. Again, outside the typical “first month” window. If your neurologist doesn’t ask about timing, they might miss it. And then there’s drug-induced hepatitis. For most drugs, liver damage shows up around 42 days after starting. But some people take months. The FDA says any reaction within 30 days should raise red flags. But if it hits at day 80? That’s still possible. It’s called idiosyncratic-meaning your body reacts oddly, and no one can predict it. That’s why doctors need to keep an open mind.What You Can Do: Tracking Your Timeline
You don’t need to be a scientist to use this knowledge. Here’s how to protect yourself:- Write down the start date of every new medication. Keep it in your phone or a notebook.
- Track symptoms with dates. Not just “I feel tired,” but “Tired since day 5.”
- Know the common windows for your drug. Google it: “[Drug name] side effect onset time.”
- Don’t assume it’s normal if symptoms appear after two weeks. That’s not “just adjusting.” It might be the drug.
- Bring your timeline to your doctor. Say: “I started this on [date], and [symptom] started on [date]. Is that typical?”

How Technology Is Changing the Game
Hospitals are starting to use AI to spot these patterns. Mayo Clinic rolled out a system in 2022 that flags potential drug reactions based on timing. Since then, they’ve caught 22% more adverse events. That’s not magic. It’s math. The system knows that if someone gets a rash 12 days after starting a new antibiotic, it’s likely related. If they get it 12 months later? Probably not. The FDA’s Sentinel Initiative now analyzes 47 million patient records to build drug-class-specific TTO baselines. That means in the future, your electronic health record might auto-alert your doctor: “Patient started metformin on Jan 10. Dizziness reported on Jan 15. 87% of similar cases show this as a known early reaction.” Even wearables are getting involved. Johnson & Johnson is testing smart patches that track glucose levels and sleep patterns for diabetes patients. If blood sugar drops suddenly three days after starting a new insulin, the system can flag it as a possible reaction-before you even feel dizzy.What’s Not Covered (And Why You Should Still Be Careful)
TTO patterns are powerful-but not perfect. They’re based on groups of people. Your body is unique. Genetics, age, liver function, other meds, even gut bacteria can change how fast a drug affects you. Also, reactions that happen after you stop the drug? They’re rarely reported. Studies show adverse events are 37% less likely to be noticed or recorded once you’ve quit the medication. So if you had a rash two weeks after stopping an old antibiotic, your doctor might never know. And no, timing doesn’t prove causation. Just because a headache started after you took a pill doesn’t mean the pill caused it. That’s why experts like Dr. David Healy warn against over-relying on TTO alone. It’s a clue-not a verdict.Final Takeaway: Be the Detective
Medications save lives. But they also come with hidden clocks. The side effect you think is “just part of getting older” might be tied to a pill you started six weeks ago. The fatigue you blame on stress could be from a drug you’ve been on for four months. You don’t need to memorize every TTO window. But you do need to know this: timing matters. Track your start dates. Note your symptoms. Ask questions. If something feels off, and it lines up with a known pattern, say something. You’re not being paranoid. You’re being informed. The future of medicine isn’t just about new drugs. It’s about understanding when they act-and when they harm. You’re not just a patient. You’re the first line of defense.How soon do side effects usually start after taking a new medication?
Most side effects appear within the first few days to weeks. About 78% of adverse reactions happen early, often within the first week. But some, like certain types of nerve damage or liver issues, can take months to show up. The timing depends on the drug class-antibiotics like ciprofloxacin often cause reactions in 2 days, while drugs like interferon beta-1a may take over a year.
Can a medication cause side effects even after you stop taking it?
Yes, but these reactions are harder to detect and often go unreported. Some drugs stay in your system for days or weeks after you stop, especially if they have a long half-life. Others trigger immune responses that linger. For example, some people develop delayed angioedema from ACE inhibitors weeks after discontinuing the drug. Because symptoms appear after stopping, doctors rarely connect them to the medication.
Are statins really responsible for muscle pain?
Not always. A major 2021 study found that patients taking statins and those taking placebo reported muscle pain at nearly the same rate. When people stopped either the real drug or a sugar pill, over half felt better within three days. This suggests a strong nocebo effect-expecting side effects can make you feel them. That doesn’t mean statins are harmless, but many cases of “statin myopathy” aren’t actually caused by the drug.
What drug has the longest known time-to-onset for side effects?
Interferon beta-1a, used to treat multiple sclerosis, has one of the longest known time-to-onset patterns for peripheral neuropathy-median of 526.5 days, or about 18 months. Other drugs like natalizumab can cause nerve damage after 141 days (nearly 5 months). These delays make diagnosis difficult because patients and doctors often don’t link symptoms to a drug taken months earlier.
Can electronic health records help detect side effects based on timing?
Yes. Systems like Mayo Clinic’s TTO-based alert tool flag potential drug reactions by matching symptom onset with known patterns. Since launching in 2022, they’ve improved adverse event detection by 22%. The FDA’s Sentinel Initiative also uses AI to analyze millions of records and build drug-class-specific timing profiles. These tools help doctors spot patterns humans might miss.







Harsh Khandelwal
December 23, 2025 AT 23:04So let me get this straight - big pharma knows exactly when their drugs turn you into a walking zombie, but they don't tell you? 🤔 I'm just saying, if your liver starts screaming at day 42, maybe the 'natural healing' ad they paid for on Instagram should've mentioned that. #DrugClockIsALie
Lindsey Kidd
December 24, 2025 AT 04:24This is SO needed!! 🙌 I started gabapentin and thought my brain fog was just 'adulting'... turns out it was day 17. Now I track everything in my Notes app. If you're on meds, DO THIS. You're not crazy - timing matters! 💊📆
Rachel Cericola
December 25, 2025 AT 07:40Let’s be real - the nocebo effect is real, but dismissing statin myopathy as ‘all in your head’ is dangerously reductive. I’ve seen patients with CK levels 12x normal and doctors still say ‘it’s probably stress.’ The data here is solid: track onset, document symptoms, demand lab work. This isn’t anecdotal - it’s evidence-based medicine. If your doctor doesn’t take timing seriously, find one who does. Your muscles aren’t drama queens.
Blow Job
December 25, 2025 AT 10:51I’m not a doctor, but I’ve been on 17 different meds since 2018. The one thing I learned? Write down the day you start. I had a rash on day 9 after starting a new blood pressure pill. Doctor said ‘allergy.’ I said ‘check the TTO chart.’ He looked it up. Turned out it was a known 7–14 day reaction. I saved myself a trip to the ER. This post? Gold.
Christine Détraz
December 26, 2025 AT 20:16I really appreciate how this breaks down the timeline instead of just saying 'side effects can happen.' It’s like knowing when your phone battery dies - if you know it drains faster after 8 hours, you don’t panic at hour 7. Same with meds. I’ve started keeping a little log in my wallet. Small habit. Big difference.
Bhargav Patel
December 27, 2025 AT 14:27The temporal dimension of pharmacological action reveals a profound epistemological gap in contemporary medical practice. While the reductionist model privileges immediate causality, the latency of idiosyncratic reactions challenges the very notion of linear causation. One must therefore adopt a hermeneutic approach - interpreting symptoms not as discrete events, but as temporal signatures inscribed upon the body by chemical agents. The patient, in this light, becomes not merely a recipient of treatment, but a living chronicle of pharmacodynamic history.
Joe Jeter
December 28, 2025 AT 16:08Funny how they say '78% happen early' - but never mention that the other 22% are the ones that kill you. And of course, the FDA doesn’t want you to know that most of these 'patterns' are based on clinical trials with 300 people who didn’t have kidney disease, diabetes, or a cat named Frank. This is corporate science dressed up like a textbook.
Sidra Khan
December 28, 2025 AT 19:00Okay but why do we only hear about the drugs that cause nerve damage? What about the ones that make you gain 40 lbs and cry uncontrollably for 3 months? Nobody talks about that. And why is it always 'track your symptoms' like it's your job now? I just want to take my pill and not become a medical detective.
Lu Jelonek
December 30, 2025 AT 01:42In my culture, we don’t always speak up about side effects - it’s seen as complaining. But this post made me realize: if I don’t say something, no one will connect the dots. I started metformin and had bloating for weeks. Thought it was my diet. Now I know it’s common in the first 4 weeks. I told my doctor. She adjusted my dose. Thank you for normalizing this.
Ademola Madehin
December 31, 2025 AT 22:03I took cipro and my foot went numb on day 2. I went to the ER. They laughed. Said 'it's probably anxiety.' I cried in the parking lot. Then I found this exact article. Now I scream it from the rooftops. This isn't just info - it's survival. My foot still tingles. But I'm alive. And I'm not quiet anymore.
siddharth tiwari
January 2, 2026 AT 11:01they got us all hooked on pills and now they want us to be doctors too?? lol. i took zoloft and got dizzy on day 5. doc said 'its normal' but i knew. they dont want you to know it takes 6 months to flush out. they make money off you staying on it. #shadowpharma
suhani mathur
January 3, 2026 AT 21:56Oh wow, so the 'just give it time' advice? Yeah, that’s just a fancy way of saying 'we don’t have data for you.' I started pregabalin, got dizzy on day 3, and my doctor said 'it’ll pass.' It didn’t. I stopped. I’m fine now. Funny how the internet knows more than my 12-minute appointment. 🙃
Diana Alime
January 5, 2026 AT 09:45i started taking the new antidepressant and my hair started falling out after 3 weeks. i thought i was just stressed. then i read this and looked it up - turns out it's a known delayed reaction. i went back to my doc and they were like 'oh yeah, that's rare.' WELL IT HAPPENED TO ME. so stop saying 'rare' like it makes it okay.
Adarsh Dubey
January 7, 2026 AT 02:38I like how this doesn’t just list drugs - it gives you a framework. I’m not a medical person, but now I know to ask: 'When does this usually start?' instead of 'Is this normal?' Small shift. Huge difference. I’ve started sharing this with my mom. She’s on 5 meds. She didn’t even know to track dates.