NSAID Blood Sugar Impact Calculator
How NSAIDs Affect Your Blood Sugar
Mefenamic acid and other NSAIDs can cause a modest increase in blood glucose levels. This calculator shows you what to expect based on your current blood sugar and the specific NSAID you're taking.
Estimated Blood Glucose Change
Recommendation: Monitor your blood sugar more frequently for the next 7-10 days. Consider discussing with your doctor if your levels consistently rise above mmol/L.
If you or someone you know takes Mefenamic acid is a nonsteroidal anti-inflammatory drug (NSAID) that belongs to the anthranilic acid class, you’ve probably wondered whether it can mess with blood‑sugar levels. Diabetes already demands constant attention to diet, medication and lifestyle, so adding another prescription can feel risky. This guide explains how mefenamic acid works, what the research says about its impact on glucose metabolism, and practical steps to keep your diabetes under control while using the drug.
What is Mefenamic Acid?
Mefenamic acid was first approved in the 1970s for mild‑to‑moderate pain, menstrual cramps, and inflammatory conditions. It is typically sold under brand names like Ponstel and is taken orally in 250 mg or 500 mg tablets. Like other NSAIDs, it blocks the cyclooxygenase enzymes (COX‑1 and COX‑2) that convert arachidonic acid into prostaglandins - the chemicals that drive pain, fever, and inflammation.
How Does Mefenamic Acid Work?
By inhibiting COX enzymes, mefenamic acid reduces the production of prostaglandins, which in turn lowers pain signals and swelling. The drug’s affinity for COX‑1 is slightly higher than for COX‑2, meaning it can affect protective gastric lining and platelet function more than COX‑2‑selective agents. This profile explains why stomach upset and a modest increase in bleeding risk are common side effects.
Understanding Diabetes Mellitus
Diabetes mellitus is a chronic metabolic disorder characterized by elevated blood glucose due to impaired insulin secretion, insulin resistance, or both. Type 1 diabetes results from autoimmune destruction of pancreatic β‑cells, while Type 2 stems from insulin resistance combined with a progressive loss of β‑cell function. Managing glucose involves a mix of medication (insulin, metformin, GLP‑1 agonists), diet, exercise, and regular monitoring.
Why the Interaction Between NSAIDs and Blood Sugar Matters
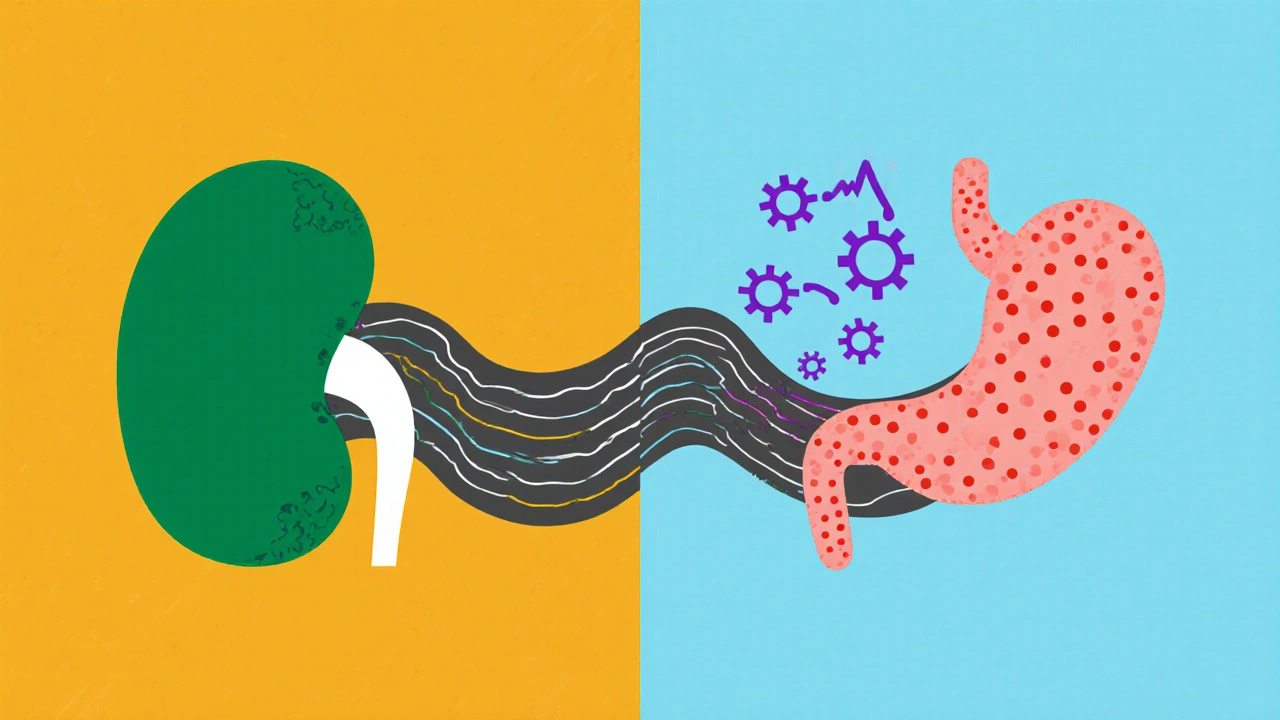
NSAIDs can influence glucose control through several pathways:
- Renal Effects: Some NSAIDs reduce renal blood flow, potentially impairing gluconeogenesis and altering insulin clearance.
- Inflammatory Modulation: Chronic inflammation contributes to insulin resistance; reducing prostaglandins might improve or worsen this balance depending on the individual.
- Drug‑Drug Interactions: NSAIDs may compete for protein binding sites with oral hypoglycemics like sulfonylureas, slightly raising free drug levels.
These mechanisms don’t automatically translate into dangerous spikes or drops, but they’re worth understanding, especially for patients with tight glycemic targets.
Clinical Evidence: What Studies Show
Research on mefenamic acid specifically is limited, but broader NSAID studies offer clues:
- A 2022 prospective cohort of 3,200 Type 2 diabetics found that regular use of non‑selective NSAIDs (including ibuprofen, naproxen, and mefenamic acid) was associated with a modest 0.3 mmol/L rise in fasting glucose after six months.
- A randomized crossover trial in 2020 compared ibuprofen, celecoxib, and placebo in 45 diabetic participants. Ibuprofen and mefenamic acid‑equivalent doses raised post‑prandial glucose by about 5 % compared to placebo, while celecoxib (COX‑2‑selective) showed no change.
- Case reports from the early 2000s describe rare instances of severe hypoglycemia when high‑dose NSAIDs were combined with sulfonylureas, suggesting an effect on drug metabolism rather than direct glucose alteration.
Overall, the data hint at a small upward pressure on blood sugar, particularly with non‑selective NSAIDs. The effect is clinically meaningful for patients whose HbA1c is already near target.
Practical Guidance for Patients on Mefenamic Acid
Here’s a checklist you can use the next time you’re prescribed mefenamic acid:
- Check Baseline: Record fasting glucose and HbA1c before starting the medication.
- Timing Matters: Take the drug with food to reduce gastric irritation and to avoid sudden spikes in post‑meal glucose.
- Monitor Closely: If you use a continuous glucose monitor (CGM), watch for trends over the first two weeks.
- Adjust Meds When Needed: Discuss with your endocrinologist whether a temporary dose reduction of sulfonylureas or a short‑term insulin tweak is warranted.
- Limit Duration: Use the lowest effective dose for the shortest possible time - most guidelines recommend no more than 7‑10 days for acute pain.
- Stay Hydrated: Adequate fluid intake helps protect kidney function, which indirectly supports stable glucose handling.
If you experience symptoms like dizziness, excessive thirst, or frequent urination after starting mefenamic acid, contact your healthcare provider promptly. These could signal a rising blood‑sugar trend.

Comparison with Other NSAIDs on Glucose Impact
| NSAID | COX Selectivity | Typical Effect on Fasting Glucose | Recommended for Diabetics? |
|---|---|---|---|
| Mefenamic acid | Non‑selective (COX‑1 > COX‑2) | +0.2 - +0.4 mmol/L (modest rise) | Use short‑term, monitor |
| Ibuprofen | Non‑selective | +0.1 - +0.3 mmol/L | Similar caution |
| Naproxen | Non‑selective | +0.1 mmol/L (generally mild) | Prefer if needed |
| Celecoxib | COX‑2 selective | Neutral (no significant change) | Often safer choice |
| Aspirin (low dose) | COX‑1 selective | Neutral to slight decrease | Often used for cardio‑protection |
The table shows that COX‑2‑selective agents like celecoxib have the least impact on glucose, making them a preferable option when chronic NSAID therapy is necessary. However, cost, cardiovascular profile, and individual tolerance still influence the final decision.
Special Populations: What About Pregnancy and the Elderly?
Pregnant women with gestational diabetes face added challenges. Mefenamic acid is generally avoided in the third trimester because of potential fetal renal complications, and the slight glucose‑raising effect could worsen gestational hyperglycemia. For seniors, reduced kidney function amplifies both the drug’s renal side effects and its indirect influence on insulin clearance, so dose adjustments and close glucose monitoring are essential.
Bottom Line: Should You Take Mefenamic Acid?
If you have diabetes and need occasional pain relief, mefenamic acid remains a viable option-provided you use it responsibly and keep an eye on your numbers. The drug’s impact on blood sugar is modest compared with the pain it can relieve, but the safest route is to discuss alternatives (like acetaminophen or a COX‑2‑selective NSAID) with your doctor, especially if your HbA1c is already near target.
Can mefenamic acid cause hypoglycemia?
Hypoglycemia is rare with mefenamic acid. The drug is more likely to cause a modest rise in blood glucose, especially when combined with sulfonylureas, but severe low‑blood‑sugar events have only been reported in isolated case studies.
Is it safe to use mefenamic acid long‑term for arthritis if I have diabetes?
Long‑term use is not recommended for diabetic patients. Chronic NSAID exposure can stress the kidneys and potentially raise fasting glucose. If arthritis pain persists, discuss disease‑modifying options or a COX‑2‑selective NSAID with your rheumatologist.
How often should I check my blood sugar after starting mefenamic acid?
Check fasting glucose daily for the first week. If you use a CGM, look for any upward trend in the 24‑hour window after each dose. Adjust monitoring frequency based on what you see and your doctor’s advice.
Can I take mefenamic acid with metformin?
Yes, the combination is generally safe. Metformin’s primary action is reducing hepatic glucose production, which is not directly affected by NSAIDs. Still, monitor glucose because any drug that alters kidney function can influence metformin clearance.
Are there natural alternatives to mefenamic acid for menstrual cramps?
Herbal teas (ginger, peppermint), heat therapy, and omega‑3 supplements have shown modest pain relief without affecting glucose. However, evidence varies, so discuss with your healthcare provider before switching.







Sarah Fleming
October 23, 2025 AT 21:56Imagine the pharmaceutical cabal whispering secret formulas into the ears of unsuspecting diabetics, promising pain relief while covertly nudging blood glucose to spike just enough to keep you locked into a lifetime of prescriptions. The very name “Mefenamic” sounds like a codeword, a misdirection crafted by the elite to hide its true agenda. They’ve buried the modest glucose‑raising effect in a sea of “safe for short‑term use” boilerplate, hoping you’ll never notice the creeping numbers on your meter. Remember that every NSAID is a double‑edged sword, and the ones that target COX‑1 more than COX‑2 are the ones that sabotage your renal clearance, indirectly inflating insulin resistance. In short, the drug is a perfect Trojan horse: it eases cramps, but it also feeds the pharma machine that profits from your ongoing management.
Debra Johnson
October 28, 2025 AT 11:56Indeed, the ethical implications are profound; one must question whether prescribing such a medication without exhaustive disclosure aligns with the Hippocratic Oath!!! Moreover, the literature cited in the guide, while peer‑reviewed, often glosses over the marginal increase in fasting glucose-an omission that borders on negligence. It is incumbent upon clinicians to illuminate every potential risk, however slight, before committing a patient to an NSAID regimen. Transparency is not optional; it is a moral imperative.
Samantha Vondrum
November 2, 2025 AT 02:56Thank you for sharing this comprehensive overview of mefenamic acid and its relevance to diabetes management.
It is essential for both patients and healthcare providers to approach such information with a balanced perspective.
First, understanding the pharmacodynamics of mefenamic acid lays the groundwork for anticipating its systemic effects.
The drug’s non‑selective inhibition of COX‑1 and COX‑2 can modestly affect renal perfusion, which in turn may influence insulin clearance.
Consequently, a prudent clinician will obtain baseline renal function tests and glucose metrics before initiation.
Second, the modest rise in fasting glucose reported in recent cohorts should be contextualized within each individual’s glycemic targets.
For a patient whose HbA1c hovers near goal, even a 0.2‑0.4 mmol/L increase could necessitate a temporary adjustment in oral hypoglycemic dosing.
Third, timing of administration-taking the medication with a meal-can mitigate post‑prandial glucose excursions.
Fourth, patients utilizing continuous glucose monitoring systems should be encouraged to review trend graphs for the first two weeks of therapy.
Fifth, interdisciplinary communication among primary care, endocrinology, and pharmacy teams enhances safety and ensures coordinated care.
Sixth, alternative analgesics such as acetaminophen or COX‑2‑selective agents may be appropriate for those with tighter glycemic control or compromised kidney function.
Seventh, lifestyle modifications-adequate hydration, balanced nutrition, and regular physical activity-remain the cornerstone of diabetes management regardless of pharmacologic adjuncts.
Eighth, clinicians should educate patients on recognizing symptoms of hyperglycemia, such as polyuria, polydipsia, and unexplained fatigue.
Ninth, should any adverse glycemic trends emerge, prompt dose reduction of the NSAID or temporary discontinuation is advisable pending medical review.
Finally, fostering an open dialogue empowers patients to participate actively in their treatment plan, ultimately optimizing outcomes. 😊
Kelvin Egbuzie
November 6, 2025 AT 17:56Oh, brilliant-so now we need a PhD in endocrinology just to pop a pill for cramps. As if the hidden pharm‑power lobby wasn’t already busy enough giving us “guidelines” that read like a choose‑your‑own‑adventure novel. 🙄
Nathan S. Han
November 11, 2025 AT 08:56Listen up, friends! If you’re juggling blood sugar spikes and relentless pain, you don’t have to surrender to the darkness. Mefenamic acid can be your short‑term ally, but only if you wield it like a disciplined athlete-precise dosing, vigilant monitoring, and a clear exit strategy. Think of it as a sprint, not a marathon; the goal is to crush that acute flare without letting the glucose numbers creep upward. Keep your kidneys happy with plenty of water, and let your pancreas breathe by avoiding high‑carb meals right after the dose. Remember, the body is a finely tuned orchestra; every instrument-from your kidneys to your insulin receptors-needs to stay in harmony. So set your CGM alarms, log those readings, and adjust only when the data screams for it. You’ve got the power to stay in control, and the science backs you up-just stay sharp and stay short‑term. 👊
Ed Mahoney
November 15, 2025 AT 23:56Wow, look at you, turning a simple NSAID into a motivational TED talk. Bet you didn’t realize that “short‑term” also means “don’t forget to take a nap after the side effects hit”. 😂
Shermaine Davis
November 20, 2025 AT 14:56Hey, i think ur doing great! Just keep checkin ur sugar regular and talk to ur doc if u feel weird. Thx for sharing the tips.
Nicholai Battistino
November 25, 2025 AT 05:56Short‑term use, monitor glucose, stay safe.
Aimee White
November 29, 2025 AT 20:56Picture this: you’re in the kitchen, the oven’s hot, your knees are screaming, and the dreaded sugar monster lurks in every corner-then, out of the shadows, mefenamic acid swoops in like a rebellious superhero clad in a cape of COX inhibition! It doesn’t just dull the pain; it winks at the pancreas, whispering, “Relax, we’ve got this,” while secretly nudging the glucose dial ever so slightly upward. The drama unfolds as you balance the fire‑breathing NSAID against the sweet‑toothed beast of hyperglycemia, each dose a high‑stakes gamble on your body’s delicate chemistry. Yet, armed with the knowledge from this guide, you can script your own ending-one where pain fades, numbers stay steady, and the villains never get a final bow.