When the pandemic hit in early 2020, most people worried about masks, ventilators, and hospital beds. But behind the scenes, something just as dangerous was unfolding: drug shortages. Essential medicines - from antibiotics to insulin to blood pressure pills - started disappearing from shelves. At the same time, illegal drug supplies became more dangerous as fentanyl crept into street drugs. For patients, this wasn’t just an inconvenience. It was life-or-death.
Why Did Medications Vanish Overnight?
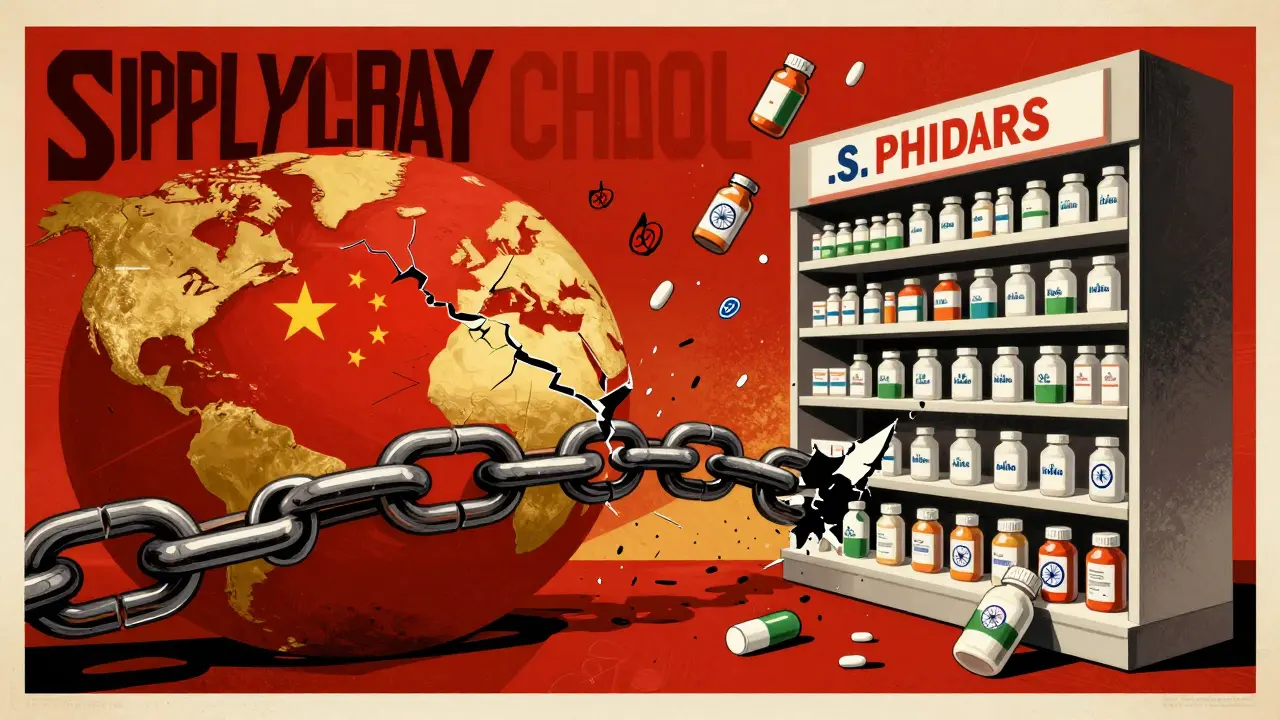
The global supply chain for pharmaceuticals was already fragile. Most active ingredients for common drugs came from just two countries: China and India. When lockdowns hit those regions in early 2020, factories slowed or shut down. Shipping ports clogged. Workers got sick. The result? A sudden, massive drop in the production of raw materials needed to make medicines. A study published in JAMA Network Open found that between February and April 2020, nearly one-third of all reported drug supply issues turned into actual shortages. That’s a fivefold increase compared to pre-pandemic levels. Drugs like propofol (used in ICU sedation), heparin (a blood thinner), and even simple antibiotics like amoxicillin became hard to find. Hospitals rationed doses. Pharmacies limited refills. Patients with chronic conditions had to switch medications - sometimes with risky side effects. The good news? After May 2020, things started to stabilize. The FDA stepped in, pushing manufacturers to report shortages earlier and fast-tracking inspections. By mid-year, the rate of new shortages dropped back to near-normal levels. But the damage was done. Many of these disruptions exposed deep flaws in how the world makes and moves medicine.Illicit Drugs Got Deadlier
While prescription drugs vanished, illegal drug markets didn’t collapse - they got more dangerous. With borders closed and traditional supply routes cut, drug cartels turned to cheaper, more potent substances. Fentanyl, a synthetic opioid 50 to 100 times stronger than morphine, became the go-to filler. It’s cheap to produce and easy to mix into heroin, cocaine, or even fake pills made to look like oxycodone. The numbers are chilling. From May 2020 to April 2021, over 97,000 Americans died from drug overdoses - a 31% jump from the year before. In states like West Virginia and Kentucky, overdose deaths rose by more than 50%. People who used drugs weren’t using more - they were just getting poisoned by what they bought. One Reddit user in the r/opiates community wrote in June 2020: "I took a dose that used to be fine and passed out for hours. Turned out it was laced with fentanyl. I got lucky. My friend didn’t." Harm reduction programs tried to respond. Needle exchanges in cities like Philadelphia and Boston started handing out naloxone - the overdose-reversal drug - at double the rate. Drive-through testing and take-home kits became common. But these efforts couldn’t keep up with the scale of the problem.Telehealth Helped - But Left People Behind
On the treatment side, the pandemic forced a massive shift to telehealth. For people with opioid use disorder, that meant doctors could prescribe buprenorphine over video calls instead of requiring in-person visits. Before the pandemic, only about 13% of these prescriptions were done remotely. By April 2020, that number jumped to 95%. That change saved lives. A study cited by the National Institute on Drug Abuse found that Medicare beneficiaries who accessed telehealth for addiction treatment were less likely to die from an overdose. For people in rural areas, it meant no more driving hours to see a specialist. For those with mobility issues or childcare responsibilities, it removed major barriers. But not everyone benefited. Older adults struggled with technology. People without reliable internet or smartphones couldn’t join virtual therapy sessions. Rural clinics lacked the staff to manage the new systems. And while telehealth expanded access to medication, it didn’t replace the human connection that recovery often needs. Group meetings, peer support, and in-person counseling dropped by 75% in the first few months of lockdowns. Many people slipped through the cracks.
Who Got Hit Hardest?
The pandemic didn’t affect everyone equally. Low-income communities, people of color, and those without health insurance faced the worst outcomes. In places with fewer pharmacies, drug shortages lasted longer. In neighborhoods with high overdose rates, fentanyl-laced drugs spread faster. People with mental health conditions were especially vulnerable. With therapy canceled and support groups shut down, many turned to drugs to cope. The CDC found that emergency room visits for drug overdoses spiked in the summer of 2020 - right when isolation and anxiety peaked. Even the data was messy. The National Survey on Drug Use and Health changed its methods in 2020 to accommodate lockdowns, making it hard to compare results with previous years. That meant public health officials were flying blind in some areas, trying to respond to a crisis they couldn’t fully measure.What’s Still Broken?
Yes, drug shortages returned to pre-pandemic levels after mid-2020. But that doesn’t mean the system is fixed. The same vulnerabilities still exist. Most generic drugs are made overseas. Manufacturers have little incentive to keep extra stock on hand - it’s cheaper to produce just-in-time. One supply chain hiccup - a power outage, a labor strike, a natural disaster - can still trigger a nationwide shortage. The overdose crisis, meanwhile, has only gotten worse. In 2022, over 107,000 Americans died from drug overdoses - the highest number ever recorded. Fentanyl is now the leading cause of death for adults between 18 and 45 in the U.S. The problem isn’t just availability - it’s safety. People need clean, reliable access to treatment, not just more pills.






kenneth pillet
January 19, 2026 AT 07:26I've been on blood pressure meds for 10 years. Last year my pharmacy ran out for 3 weeks. They gave me a different brand and my head started spinning. Had to go to urgent care. No one warned me.
Just saying - this isn't abstract. It's real life.
Jodi Harding
January 19, 2026 AT 23:06Fentanyl isn't the problem. The system is. We let corporations decide who lives and who dies. And now we're surprised when people die?
Danny Gray
January 21, 2026 AT 14:04Interesting how everyone blames China and India but never mentions the FDA's own regulatory delays. You want supply chain security? Stop making companies wait 18 months to approve a new generic. That's the real bottleneck.
Also, why is no one talking about how the DEA's quota system for buprenorphine made access worse? Just saying.
Zoe Brooks
January 22, 2026 AT 06:01I work at a community pharmacy. We handed out over 200 naloxone kits last year. People don't come in asking for them. They just take them. Quietly. Gratefully.
It's not glamorous. But it saves lives. We need more of this. Not more policing.
Wendy Claughton
January 22, 2026 AT 11:21I just want to say thank you to the pharmacists, harm reduction workers, and telehealth providers who showed up when no one else did. You were the quiet heroes. And you didn't get medals. You got exhaustion, burnout, and thank-you notes on sticky notes.
It matters. I see you. ❤️
Stacey Marsengill
January 23, 2026 AT 15:40Of course the rich are fine. They have private doctors who fly in IV antibiotics from Switzerland. Meanwhile, my cousin's diabetic aunt had to split her insulin vial in half because the refill was 'delayed'.
That's not a shortage. That's a death sentence with bureaucracy.
Aysha Siera
January 24, 2026 AT 13:21You think this was an accident? 5G towers, Bill Gates vaccines, and now drug shortages? All part of the Great Depopulation. The same people who control the FDA control the factories. They want you weak. Dependent. Controlled.
Selina Warren
January 24, 2026 AT 23:45Telehealth saved my life. I live in rural Ohio. Before 2020, I drove 3 hours every week for a buprenorphine script. Now I get it from my couch. No judgment. No waiting. Just medicine.
Don't let them take it away.
Emma #########
January 26, 2026 AT 16:37I lost my dad to an overdose in 2021. He never knew his pills were laced. He just thought he was taking his usual pain med. We found a test strip in his pocket. He tried. He really tried.
Just... thank you for writing this.
Andrew McLarren
January 27, 2026 AT 21:17The structural vulnerabilities in the pharmaceutical supply chain were well documented prior to the pandemic. The failure to implement risk mitigation strategies constitutes a systemic governance deficiency. One might argue that the prioritization of cost-efficiency over resilience represents a misalignment of public health imperatives with market-driven logic.
Andrew Short
January 28, 2026 AT 10:04People died because they were too lazy to get off drugs. The real crisis is moral decay. Why are we spending millions on naloxone instead of telling addicts to get a job and stop being weak?
christian Espinola
January 29, 2026 AT 15:35The article mentions FDA fast-tracking inspections. But it fails to cite the 2021 GAO report showing that 68% of those inspections were conducted remotely due to staffing shortages. Meaning: the FDA approved drugs without ever seeing the facility. That's not oversight. That's negligence.