Isotretinoin Dose Calculator
Calculate Your Isotretinoin Dosage
Isotretinoin is typically prescribed at 0.5–1 mg per kilogram of body weight per day, taken for 4–6 months.
Why the debate matters
Severe acne can feel like a never‑ending battle, and the choice of medication often feels like a high‑stakes gamble. On one side you have Isotretinoin an oral retinoid known for delivering dramatic, long‑lasting clearance. On the other, a mix of topical agents, oral antibiotics and hormone‑based pills promise milder results with fewer risks. This guide breaks down the science, the side‑effects, and the real‑world pros and cons so you can decide which route fits your skin (and lifestyle) best.
What Is Isotretinoin?
Isotretinoin is a synthetic derivative of vitamin A, classified as a systemic retinoid. It works by shrinking the sebaceous glands, reducing sebum production, normalising skin cell turnover, and dampening the inflammatory response that fuels acne lesions. Because it attacks the four major causes of acne-excess oil, clogged pores, bacteria and inflammation-it’s often the go‑to for nodular or cystic acne that hasn’t responded to other therapies.
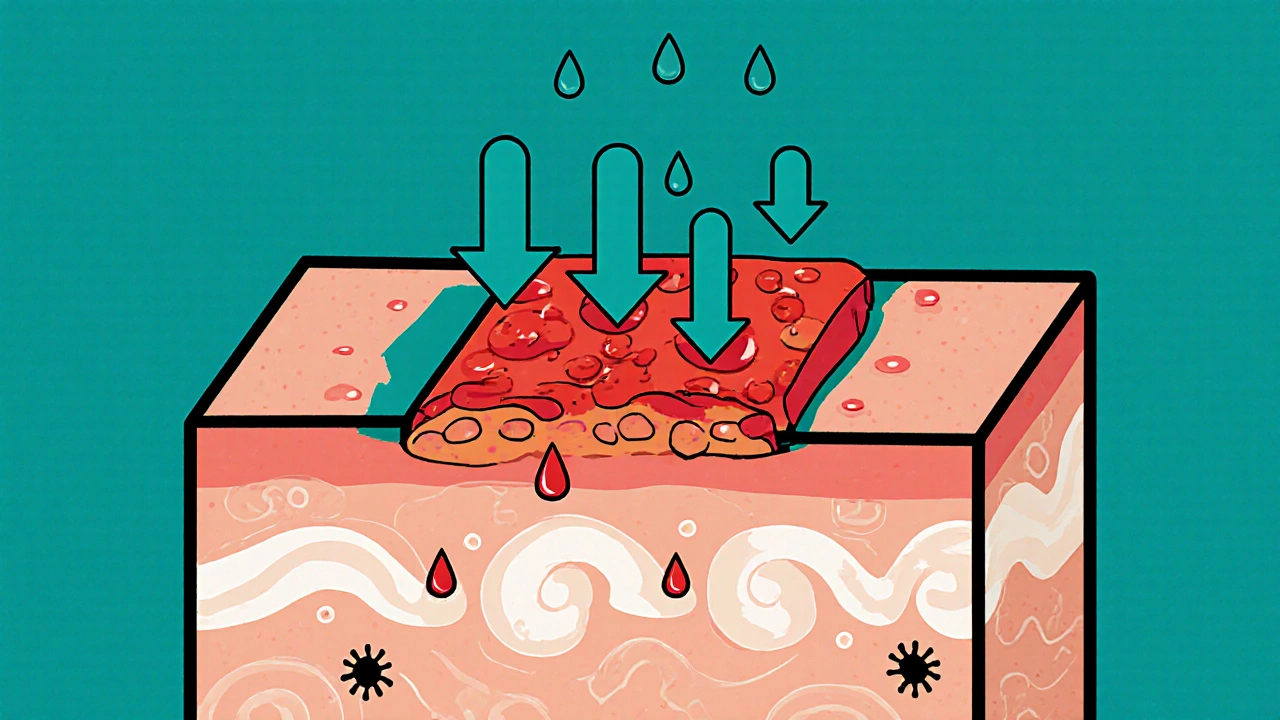
How It Works: The Mechanism in Plain English
- Sebum suppression: Glands shrink by up to 70%, cutting the oily fuel for bacteria.
- Cell turnover: Skin cells shed more evenly, preventing blockages that turn into blackheads.
- Anti‑inflammatory action: Reduces the redness and swelling that make lesions painful.
- Anti‑bacterial effect: By starving Cutibacterium acnes, it curbs bacterial overgrowth indirectly.
The result is a gradual, but often dramatic, reduction in both active lesions and future breakouts.
Typical Treatment Regimen and Benefits
Doctors usually prescribe a dose that equals 0.5-1 mg per kilogram of body weight per day, taken for 4-6 months. Most patients see a 50-80 % drop in lesion count after the first two months, and many enjoy clearance that lasts years after stopping the drug.
Key benefits include:
- Long‑term remission for severe cases.
- Resolution of deep cysts that can scar.
- Improved self‑esteem and quality of life.
Side‑Effects and Safety Precautions
Because isotretinoin hits the whole body, it carries a heavier side‑effect profile than most topical or oral alternatives.
- Dry skin and lips: Almost every patient needs a good lip balm.
- Elevated triglycerides and liver enzymes: Regular blood tests are mandatory.
- Birth‑defect risk: Pregnancy must be avoided; strict contraceptive protocols are required.
- Mood changes: Some reports link isotretinoin to depression; close monitoring is advised.
If you’re a woman of child‑bearing age, a signed iPLEDGE agreement (or its Australian equivalent) is non‑negotiable.
Popular Alternatives at a Glance
Not every acne case needs isotretinoin. Below are the most frequently prescribed options, each with its own niche.
| Medication | Type | Typical Use | Effectiveness (lesion reduction) | Common Side‑Effects |
|---|---|---|---|---|
| Tretinoin | Topical retinoid | Mild‑to‑moderate comedonal acne | 30‑50 % | Dryness, irritation, photosensitivity |
| Doxycycline | Oral antibiotic | Inflammatory papules/pustules | 40‑60 % | GI upset, photosensitivity, rare esophagitis |
| Spironolactone | Anti‑androgen oral | Hormonal acne in adult women | 30‑55 % | Breast tenderness, potassium elevation, menstrual changes |
| Benzoyl Peroxide | Topical antiseptic | Mild‑to‑moderate inflammatory acne | 20‑40 % | Dryness, bleaching of fabrics, mild irritation |
| Adapalene | Topical retinoid (new‑generation) | Comedonal & inflammatory acne | 35‑55 % | Dryness, mild burning, better tolerance than tretinoin |
Choosing Between Isotretinoin and the Alternatives
Think of acne treatment like a toolbox. Isotretinoin is the hammer-effective for big, stubborn problems but requires caution. The alternatives are the screwdriver, wrench, and pliers-each handles specific tasks with less risk.
Consider isotretinoin when:
- You have nodular or cystic acne that has not improved after 3-6 months of antibiotics or topical retinoids.
- Scarring is a major concern and you need rapid, deep clearance.
- You can commit to monthly blood work and strict birth‑control measures.
Opt for alternatives when:
- Acne is mild‑to‑moderate, primarily comedonal.
- You prefer over‑the‑counter or short‑term oral options.
- You have contraindications to retinoids (e.g., pregnancy, severe liver disease).
Practical Tips for Patients on Isotretinoin
- Lab monitoring: Baseline liver function tests (ALT, AST) and lipid profile, then repeat every 4-6 weeks.
- Hydration: Use fragrance‑free moisturisers and lip balms multiple times a day.
- Sun protection: SPF 30+ broad‑spectrum sunscreen daily; isotretinoin heightens photosensitivity.
- Women of child‑bearing age: Two reliable forms of contraception, monthly pregnancy tests, and a signed risk‑management pledge.
- Psychological check‑ins: Keep a mood journal; alert your dermatologist if you feel unusually down.
Stopping the drug abruptly can cause rebound acne, so taper under medical supervision if side‑effects become intolerable.
Bottom Line: Tailor the Treatment to the Person, Not Just the Pimple
There’s no one‑size‑fits‑all cure. Isotretinoin delivers unmatched results for severe, scarring‑prone acne, but it demands a solid safety net. The alternatives-topical retinoids, oral antibiotics, hormonal agents, and benzoyl peroxide-provide respectable clearance with fewer systemic risks, making them ideal for lighter cases or for patients who cannot meet isotretinoin’s monitoring requirements.
Talk openly with a dermatologist, weigh the pros and cons listed above, and choose the path that aligns with your skin goals and lifestyle.

Can isotretinoin cause permanent side‑effects?
Most side‑effects-dry skin, lips, and elevated lipids-reverse after the course ends. Rarely, lasting joint pain or mood changes have been reported, but they’re not common. Long‑term studies show no permanent organ damage when monitoring guidelines are followed.
How long does the isotretinoin treatment last?
Typical courses run 4-6 months, aiming for a cumulative dose of about 120-150 mg/kg. Some patients need a second round if acne returns.
Is isotretinoin safe for teenagers?
Yes, provided they aren’t pregnant and can handle monthly labs. Many dermatologists start teens at the lower end of the dose range to minimise dryness.
What’s the biggest difference between isotretinoin and topical retinoids?
Isotretinoin works systemically, shrinking all sebaceous glands, while topical retinoids only affect the skin surface. Hence, oral isotretinoin can clear deep cysts, but it also brings systemic risks.
Can I use benzoyl peroxide while on isotretinoin?
A gentle, low‑strength benzoyl peroxide can help control bacteria, but many dermatologists recommend waiting until isotretinoin stabilises skin to avoid excessive irritation.







Diane Thurman
October 22, 2025 AT 17:31Isotretinoin is definetly overhyped; most people just want a quick fix and ignore the long term risks, hte side effects can be a nightmare if you’re not super careful.
Iris Joy
October 27, 2025 AT 23:54Hey folks, if you’re on the fence, remember that isotretinoin can be a game‑changer for severe cystic acne. It’s true the monitoring is a hassle, but the confidence boost after clearing those deep lesions is worth it. Start slow, hydrate your skin, and keep those lip balms handy. For milder cases, a combo of topical retinoids and benzoyl peroxide can often do the trick without the systemic load. Keep in close touch with your dermatologist and listen to your body’s signals.
Joe Waldron
November 2, 2025 AT 07:17When considering isotretinoin, note the dosage range-0.5 to 1 mg/kg/day; this allows clinicians to tailor therapy based on severity, hepatic function, and lipid profile. Regular lab work, typically every 4‑6 weeks, monitors ALT, AST, and triglycerides, mitigating potential toxicities. Additionally, patients should employ fragrance‑free moisturizers, lip balms, and broad‑spectrum SPF 30+ sunscreen, as the drug increases photosensitivity. For women of child‑bearing potential, two reliable contraceptive methods plus monthly pregnancy tests are non‑negotiable; the iPLEDGE program enforces this. Lastly, a gradual taper rather than abrupt cessation helps prevent rebound acne, preserving the gains achieved during treatment.
John Connolly
November 7, 2025 AT 14:40I see your point about the hype, but let’s not discount a medication that has helped countless people regain confidence. The rigorous monitoring is a safety net, not a barrier. If you pair the treatment with proper skin care, the side‑effects become manageable. Think of it as a partnership between you and your dermatologist, each playing a crucial role. Ultimately, the decision should balance severity, lifestyle, and personal comfort.
Sameer Khan
November 12, 2025 AT 22:03From a pharmacodynamic perspective, isotretinoin operates via modulation of the retinoic acid receptors, effectuating a cascade that culminates in sebaceous gland atrophy. This mechanistic pathway is distinct from topical retinoids, which merely influence epidermal turnover without systemic glandular suppression. Consequently, the therapeutic index is broadened, yielding a higher magnitude of lesion reduction, often exceeding 80 % in refractory nodular cases. Nonetheless, the systemic exposure predicates a spectrum of iatrogenic sequelae, necessitating vigilant hepatic function assays and lipid panel surveillance. Moreover, teratogenicity remains the paramount contraindication, thereby mandating stringent contraceptive adherence and enrollment in risk mitigation programs such as iPLEDGE. In juxtaposition, oral tetracyclines like doxycycline exert bacteriostatic activity against Cutibacterium acnes, attenuating inflammation but lacking the glandular destructuring efficacy. Hormonal agents, notably spironolactone, mitigate androgen-driven sebum production, offering a viable adjunct in female patients with hormonal dysregulation. Topical modalities-benzoyl peroxide and adapalene-provide incremental anti‑inflammatory and comedolytic effects, albeit constrained by surface‑level penetration. The clinician’s algorithm thus entails stratifying the acne phenotype, assessing comorbidity profiles, and calibrating the risk‑benefit matrix accordingly. When severe scarring potential looms, isotretinoin’s capacity for durable remission can outweigh transient adverse events, provided that adherence to monitoring protocols is uncompromised. Conversely, in mild to moderate presentations, the incremental benefit of isotretinoin may not justify the systemic burden, directing therapeutic preference toward topical or antibiotic regimens. Ultimately, a personalized therapeutic regimen, anchored in patient education and shared decision‑making, optimizes both clinical outcomes and quality‑of‑life metrics.
WILLIS jotrin
November 18, 2025 AT 05:26Honestly, it’s a bit of a trade‑off. Isotretinoin can clear up deep cysts that would otherwise scar, but you’ve got to be ready for the dryness and lab work. If you’re chill about committing to the routine, it can be worth it. Otherwise, the milder options keep things simple.
Michael Vandiver
November 23, 2025 AT 12:49👍 Isotretinoin works like a boss! 🚀
Sarah Riley
November 28, 2025 AT 20:12The isotretinoin paradigm is a toxic exemplar of pharmaceutical overreach; its adverse risk vector eclipses any marginal efficacy gains.
Tammy Sinz
December 4, 2025 AT 03:35Look, the data suggests isotretinoin is justified only for severe, scarring‑prone acne; patients with mild comedonal issues should not be subjected to such aggressive therapy. The protocol must be transparent, and the psychological monitoring should be non‑optional.
Christa Wilson
December 9, 2025 AT 10:59Stay positive! 🌟 Even if the journey feels long, the end result can be amazing. You’ve got this! 😊
Sajeev Menon
December 14, 2025 AT 18:22Hey! Just wanted to say that no matter which path you choose, consistency is key. Keep up with your labs, moisturize, and dont forget the lip balm-its choppy in the begining but you’ll get there! :)
Emma Parker
December 20, 2025 AT 01:45OMG, I totally get you! I once tried isotroeenoin and it was a rollercoaster. If you need any tips on how to survive the dryness, hit me up!
Wade Grindle
December 25, 2025 AT 09:08From a cultural standpoint, the perception of acne treatment varies globally; in some regions, oral retinoids are embraced, whereas elsewhere topical regimens dominate due to accessibility and cultural attitudes toward systemic medication.
Jai Reed
December 30, 2025 AT 16:31The comprehensive review you gave is solid, but remember that the simplest approach often wins. If a patient can’t commit to the labs, opt for a straightforward topical stack and monitor progress closely.