Every year, over 1.5 million Americans are harmed by medication errors. That’s more than car accidents or falls. And it’s not just happening in hospitals-it’s happening in kitchens, bathrooms, and living rooms where people take their pills every day. Most of these errors are preventable. But without clear systems, simple mistakes become life-threatening.
What Counts as a Medication Error?
A medication error isn’t just taking the wrong pill. It’s anything that goes wrong between when a drug is prescribed and when it’s taken. That includes:- Getting the wrong drug
- Taking the wrong dose
- Missing a dose
- Taking two drugs that shouldn’t be mixed
- Using expired or fake medicine
- Not knowing why you’re taking a pill
The World Health Organization calls this a global crisis. In the U.S. alone, medication errors cause at least one death every day. In hospitals, they’re the leading cause of preventable harm. At home, they’re quietly killing older adults who juggle five, six, or even ten pills a day.
Why Hospitals Still Get It Wrong
Hospitals have spent millions on technology to stop these errors. Barcode scanning systems (BCMA) are now standard in most U.S. hospitals. They work like this: a nurse scans the patient’s wristband and the pill’s barcode before giving a drug. If something doesn’t match-wrong drug, wrong dose, wrong time-the system stops them.It sounds perfect. And it works-when it works right. A 2025 study in JMIR found BCMA cut wrong drug errors by over 56% and missed doses by two-thirds. But here’s the catch: nurses say it adds 15 to 20 minutes to every medication round. That’s a lot when you’re managing 30 patients. So what happens? They start scanning multiple pills at once. Or they skip the scan if the barcode is smudged. Or they turn off the alerts because they’re flooded with 50 fake warnings an hour.
That’s alert fatigue. And it’s deadly. A 2024 study found 42% of clinicians ignore medication alerts just to keep moving. The system was built to protect them. But if it slows them down too much, they’ll find a way around it.
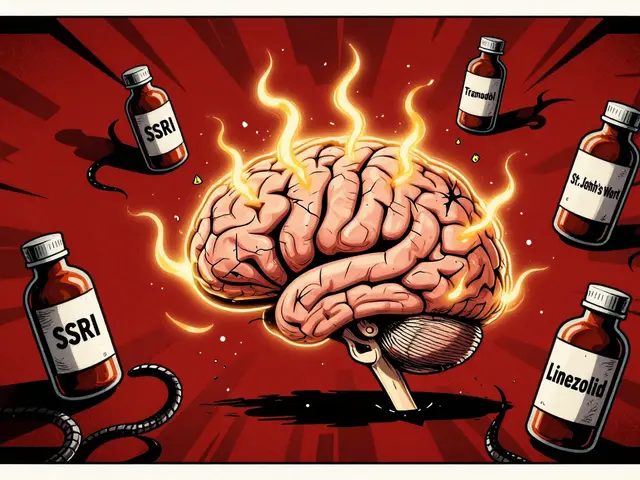
Computerized order entry (CPOE) helps too. Doctors type prescriptions instead of scribbling them on paper. That cuts down on handwriting errors. But if the system doesn’t understand the patient’s full history-like that they’re also taking St. John’s Wort or a high-dose fish oil supplement-it might miss a dangerous interaction. And if the system is clunky, doctors start using shortcuts. That’s how errors sneak back in.
The Real Problem: Transitions of Care
One of the biggest killers is what happens when patients move from one place to another. From hospital to home. From ER to rehab. From nursing home to hospice.When a patient gets discharged, their list of meds often gets messed up. The hospital might stop a blood thinner. But the home care nurse doesn’t know. Or the family doctor adds a new painkiller without checking what the hospital prescribed. The result? A 68-year-old woman ends up on three blood thinners at once. She bleeds internally. She’s back in the hospital.
Medication reconciliation-where a pharmacist sits down with the patient and compares every single pill they’ve ever taken-is the fix. But only 37% of U.S. hospitals do it well at discharge. Most just hand the patient a printout with 12 drugs listed. No explanation. No check. No follow-up.
That’s why the Joint Commission requires hospitals to do this. But requirements don’t fix broken workflows. You need trained pharmacists, time, and a system that talks to the doctor’s office. Too often, none of that exists.
Home Medication Errors Are Worse Than You Think
At home, there’s no barcode scanner. No nurse. No pharmacist double-checking. Just you, your pill organizer, and a stack of bottles.People aged 75+ who take five or more medications make up 89% of home medication errors. The most common mistake? Taking the wrong pill at the wrong time. Why? Because they have five different pill boxes. One for mornings, one for afternoons, one for nights. One for vitamins. One for supplements. And they all look the same.
A 2025 survey on SingleCare.com found 63% of seniors using pill organizers still get confused between them. They open the wrong one. Take two pills instead of one. Skip a day because they think they already took it. And they don’t tell anyone because they’re embarrassed.
Over-the-counter drugs make it worse. People take Tylenol for pain, not realizing their blood pressure pill already has acetaminophen in it. They take ibuprofen for arthritis, not knowing it’s dangerous with their heart medication. And they never tell their doctor because they think “it’s just a pill.”
What Actually Works at Home
Technology doesn’t help much at home. But simple, human-centered changes do.- Single-dose packaging: Pharmacies can pack each day’s meds into one sealed pouch. No more juggling bottles. Just open and take. Studies show this cuts home errors by 28%.
- Weekly pharmacist reviews: A pharmacist calls or visits once a week to go over the med list. They check for duplicates, interactions, and side effects. This reduces errors by 37% in seniors, according to Annals of Internal Medicine.
- One pill, one time, one reason: If you’re taking more than three meds a day, ask your doctor if you can cut it down. Many older adults are on drugs that were prescribed years ago and aren’t needed anymore.
- Use a whiteboard: Write down every medication, the dose, and why you’re taking it. Put it on the fridge. Show it to visitors. If you can’t explain why you’re taking a pill, you shouldn’t be taking it.
- Never take meds from someone else: A friend says their blood pressure pill works great? Don’t try it. Fake drugs are flooding the internet. Over 95% of online pharmacies selling prescription meds are illegal. Many use fake Canadian logos to trick you.
High-Risk Drugs Are the Deadliest
Not all meds are equal. Some are like loaded guns. One mistake and you’re in the ICU.The FDA says insulin, blood thinners like warfarin, and opioids like oxycodone cause 62% of all severe medication errors. These are called “high-alert medications.”
Insulin is especially dangerous. Too much? You go into a coma. Too little? Your blood sugar spikes, damaging your kidneys and nerves. But many people still use syringes instead of pens. They misread the lines. They reuse needles. They store it wrong.
Warfarin is another silent killer. It interacts with everything-green veggies, antibiotics, herbal teas. One wrong dose and you bleed inside your brain. Yet, many patients still get it without regular blood tests.
And opioids? They’re still overprescribed. People take them for back pain. Then they run out. Then they buy them online. Then they get fake pills laced with fentanyl. In 2024, the FDA’s MAUDE database recorded over 12,000 deaths linked to counterfeit painkillers.

The Future: AI and Blockchain
The good news? We’re getting smarter.Johns Hopkins is testing AI that predicts which prescriptions are likely to cause harm before they’re even written. In a 2024 trial, it cut high-risk prescribing errors by 53%. The system looks at your age, your other meds, your kidney function, even your recent lab results. If something’s risky, it flags it before the doctor hits send.
And blockchain? It’s not just for crypto. Hospitals in 12 states are now using it to track every pill from factory to patient. If a bottle of metformin has a fake barcode, the system knows. It can trace it back to the supplier. This could finally stop the flood of fake drugs.
But here’s the truth: technology won’t fix this alone. A 2025 ECRI report says 68% of barcode system failures happen because staff weren’t trained properly. Or the workflow didn’t change. Or leadership didn’t care.
What You Can Do Today
You don’t need a hospital system to stay safe. You just need to be proactive.- Keep a written list of every medication, supplement, and OTC drug you take. Include the dose and why. Update it every month.
- Bring it to every appointment. Don’t rely on memory. Don’t assume the doctor knows.
- Ask three questions every time you get a new prescription: What is this for? What happens if I miss a dose? What should I avoid while taking it?
- Use one pharmacy. That way, the pharmacist can see everything you’re on and catch interactions.
- Call your pharmacist if you’re confused. They’re trained to help. No judgment.
- Don’t be afraid to say no. If a doctor says you need another pill, ask: “Is this really necessary?” Many older adults are on drugs they don’t need.
Final Thought: Safety Is a Team Sport
Medication safety isn’t just about tech or rules. It’s about people. Nurses. Pharmacists. Doctors. Family members. And you.Hospitals can build better systems. But if the staff is tired, overwhelmed, or trained poorly, it won’t matter. Families can help. But if they don’t know what’s in the pill bottles, they can’t help.
Real change happens when everyone speaks up. When a nurse says, “I don’t feel right about this dose.” When a daughter says, “Mom, you’re taking two of these now?” When a patient says, “I don’t know why I’m on this.”
That’s how you stop errors. Not with scanners. Not with apps. But with courage. With questions. With care.
What’s the most common medication error at home?
The most common error is taking the wrong pill at the wrong time, especially among seniors taking five or more medications. Confusion between multiple pill organizers, missed doses, and accidental double-dosing are the top issues. Studies show 41% of home errors are due to incorrect timing, and 33% are due to wrong dosage.
Can barcode scanning really prevent medication errors in hospitals?
Yes, but only if used correctly. A 2025 study showed barcode medication administration (BCMA) reduced wrong drug errors by 56.85% and missed doses by 66.67%. However, if staff are rushed or alerts are too frequent, they bypass the system. In fact, 57% of pharmacists report new errors are being created because of workarounds.
What’s medication reconciliation, and why does it matter?
Medication reconciliation is the process of comparing a patient’s current meds with what was prescribed during a hospital stay or care transition. It’s critical because up to 70% of discharge summaries contain errors. When pharmacists do this properly, it reduces adverse drug events by up to 50%. But most hospitals don’t do it well at discharge.
Are online pharmacies safe for buying medications?
No, most are not. Over 95% of online pharmacies selling prescription drugs operate illegally. Many fake Canadian sites use maple leaf logos to trick people. These sites often sell fake, expired, or contaminated drugs-including pills laced with fentanyl. Always buy from licensed U.S. pharmacies with a physical address and a licensed pharmacist available to answer questions.
Which medications are the most dangerous if taken incorrectly?
Insulin, blood thinners like warfarin, and opioids like oxycodone are the deadliest. These are called high-alert medications. A small mistake-like taking too much insulin or mixing warfarin with certain antibiotics-can cause coma, internal bleeding, or death. They account for 62% of all severe medication errors, according to the FDA’s 2024 MAUDE database.
How can I reduce my risk of medication errors if I take multiple pills?
Use single-dose packaging from your pharmacy, keep a written and updated med list, ask your pharmacist to review your meds every 3 months, and never take a new pill without knowing why. Also, simplify your routine: if you’re on more than three daily doses, ask your doctor if any can be cut or combined. Most seniors can safely reduce their pill count by 20-30%.



Charles Barry
December 22, 2025 AT 21:57Let me guess - the hospital’s ‘barcode system’ is just another government-funded paperweight. I’ve seen it myself. Nurses scan five pills at once while scrolling TikTok. The system doesn’t stop errors - it just creates new ones. And don’t get me started on the ‘AI predictors.’ That’s just Big Pharma’s way of replacing pharmacists with algorithms that don’t even know what a ‘St. John’s Wort’ is. This isn’t healthcare. It’s a corporate simulation game where the players are dying.
Rosemary O'Shea
December 23, 2025 AT 07:34Oh, darling, how quaint. You think a barcode is the issue? The real tragedy is that we’ve outsourced basic human responsibility to machines. A nurse should be trained to *think*, not to scan. And yet, here we are - a society that treats medication like a vending machine: insert card, press button, hope for the best. The elderly? They’re not victims of bad tech - they’re victims of our collective moral laziness. We stopped caring when we stopped requiring accountability.
Sam Black
December 23, 2025 AT 14:02I’ve worked with seniors in rural Australia for over a decade. The real hero here isn’t the barcode scanner or the AI - it’s the local pharmacist who drives 40 miles once a week to sit with Mrs. Henderson and go over her meds with a highlighter and a cup of tea. She doesn’t have a digital record. She has a notebook, a memory, and the patience to listen. Tech can help, sure - but it can’t replace the quiet, stubborn act of showing up.
Tony Du bled
December 24, 2025 AT 15:03My grandma took 11 pills a day. She had four different pill boxes. One had her blood pressure meds. Another had the vitamins. The third was for the ‘extra’ stuff she bought online. The fourth? Empty. She forgot what was where. One day she took two blood pressure pills because she thought she missed one. Ended up in the ER. No one knew until the neighbor called. We need more people like the pharmacist in this post - not more apps.
Candy Cotton
December 25, 2025 AT 11:29It is entirely unacceptable that the United States, the world's preeminent leader in medical innovation, continues to tolerate such systemic incompetence. The fact that medication errors remain prevalent is not a failure of technology - it is a failure of discipline, of oversight, and of national character. We have the tools. We have the data. What we lack is the will to enforce standards. Until every nurse, every pharmacist, every physician is held to the highest possible standard of accountability, this will continue. And it is a national disgrace.
Jeremy Hendriks
December 27, 2025 AT 01:57Here’s the uncomfortable truth: we don’t fear death. We fear being forgotten. That’s why we hoard pills like talismans - because if we’re taking something, we must be doing something right. But medicine isn’t magic. It’s math. And we’ve turned it into a religion. We worship the pill, the prescription, the algorithm - but we forget the person. The body. The breath. The fear. Until we stop treating patients like data points and start treating them like people who are scared, confused, and tired - no scanner will save us.
Tarun Sharma
December 27, 2025 AT 02:37Thank you for this detailed analysis. In India, we face similar challenges, but with less infrastructure. Many elderly patients rely on family members to manage medications. Training caregivers, even with simple visual charts, reduces errors significantly. The key is clarity, not complexity. Simple systems, well-executed, outperform high-tech solutions in low-resource settings.
Gabriella da Silva Mendes
December 27, 2025 AT 15:16OK but like… why are we even talking about this? 😴 I mean, I get it, people die from meds, but like… isn’t that just the price of living in 2025? Also, I just Googled ‘best blood pressure pill’ and bought some from a site with a maple leaf. It came in a box that looked legit. 🤷♀️ Also, my cousin’s friend’s aunt took 14 pills a day and now she’s ‘vibing’ in a nursing home. So… maybe the real problem is people just shouldn’t be old? 🤔 #MedicationMystery #OverMedicatedAndOverIt
Jim Brown
December 28, 2025 AT 15:32There is a profound irony in our pursuit of perfect systems to manage human frailty. We build algorithms to predict errors, barcodes to verify doses, and blockchain to trace pills - yet we refuse to sit with the person who must take them. The soul of medicine is not in the machine’s precision, but in the silence between questions. The pause before the pill is swallowed. The hand that steadies the cup. The voice that says, ‘Do you know why you’re taking this?’ Technology can assist - but it cannot atone for the absence of presence.
Jamison Kissh
December 30, 2025 AT 10:53What if the real solution isn’t more tech, but less clutter? My grandfather took 12 pills a day. We sat down with his doctor and asked: ‘Which of these are still necessary?’ We cut it to five. Three were for conditions he didn’t even have anymore. One was a placebo from 2008. He said he felt better after stopping them. Not because of the medicine - because he stopped feeling like a pharmacy. Maybe the most powerful drug is simplicity.