Obstructive sleep apnea (OSA) isn’t just about snoring. It’s when your throat muscles relax so much during sleep that your airway collapses, stopping your breathing-sometimes dozens of times an hour. Your body jolts awake just enough to restart breathing, but you rarely remember it. The result? Exhaustion, brain fog, high blood pressure, and a much higher risk of heart attack or stroke. If you’ve been told you have OSA, you’re not alone. About 1 billion people worldwide live with it. And while CPAP therapy has been the go-to solution for over 40 years, it’s not the only option-and for many, it’s not the best one.
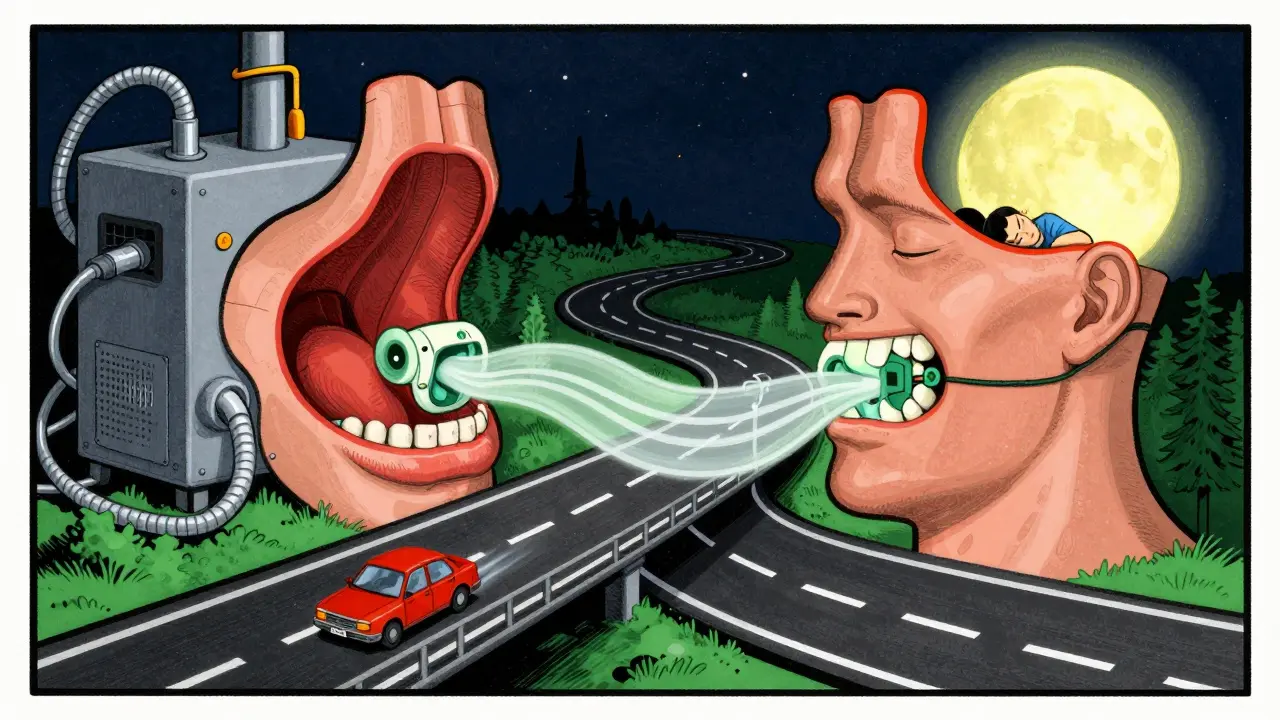
How CPAP Therapy Works
CPAP, or continuous positive airway pressure, is a machine that blows a steady stream of air through a mask you wear while sleeping. That air pressure acts like a splint, holding your airway open so you can breathe normally. It’s not magic, but it’s science that works. Developed in 1981 by an Australian doctor at the University of Sydney, CPAP became the gold standard after studies showed it could cut severe sleep apnea events from nearly 40 per hour down to under 8 with consistent use.
Modern CPAP devices come in three main types:
- Standard CPAP delivers one fixed pressure all night-usually between 6 and 12 cm H₂O.
- Auto-CPAP (APAP) adjusts pressure automatically based on your breathing. If you snore or have an event, it increases pressure. If you’re breathing smoothly, it drops it down. This is now the most common type prescribed.
- BiPAP gives two different pressures: higher when you inhale, lower when you exhale. It’s often used if you have lung issues or find CPAP uncomfortable.
Most machines weigh less than 3 pounds, make about as much noise as a whisper, and connect to apps like ResMed’s AirView or Philips DreamMapper. These apps track how many hours you use it, how many leaks you have, and whether your apnea events are dropping. Insurance companies in the U.S. require you to use it at least 4 hours a night on 70% of nights to keep coverage. About 70% of patients meet that threshold.
Why People Struggle With CPAP
CPAP works-but only if you use it. And here’s the hard truth: nearly half of people who start CPAP stop using it within a year. Why? It’s not laziness. It’s the machine itself.
- Mask discomfort is the #1 reason. Whether it’s the straps digging into your face, the cushion leaking, or the feeling of being trapped, 35% of new users quit because of this.
- Claustrophobia affects 12% of users. For them, even the smallest mask feels like suffocation.
- Mouth breathing ruins everything. If you breathe through your mouth while wearing a nasal mask, air escapes, the pressure drops, and your apnea comes back. Studies show 61.8% of people who start with nasal masks end up switching to full-face masks within six months.
- Dry nose or throat happens to 30% of users. Heated humidifiers fix this for 78% of them, but many don’t know to ask for one.
Real users say it best. One Reddit user, u/SleeplessInSeattle, wrote: “After 3 months of leaks and frustration, I switched to a nasal pillow mask. Now I sleep 7+ hours. My daytime sleepiness score dropped from 16 to 7.” Another, u/TiredButNotSleeping, said: “I’ve tried five masks over two years. Still can’t get past 2 hours. The claustrophobia is unbearable.”
Oral Appliances: The Quiet Alternative
If CPAP feels like a prison, oral appliances might be your escape. These are custom-made mouthpieces, similar to sports guards or orthodontic retainers, that shift your lower jaw slightly forward. That pulls your tongue and soft tissues away from the back of your throat, keeping your airway open.
They’re not for everyone. The American Academy of Sleep Medicine recommends them for mild to moderate OSA, or for severe cases where CPAP isn’t tolerated. But here’s the kicker: people use them way more often. A 2017 review found users wear oral appliances 77% of nights after a year. CPAP? Median use is 4 to 5 hours per night-and many use it less than 4.
Why the difference? They’re small, quiet, easy to travel with, and don’t feel invasive. One study showed four out of six patients preferred them over CPAP. The trade-off? They’re not as powerful. CPAP can bring a severe AHI (apnea-hypopnea index) down to near zero. Oral appliances typically cut it by about half. For someone with an AHI of 40, that’s still 20 events per hour-enough to cause health risks. But if you’re getting 7 hours of sleep with a mouthpiece instead of 2 hours with a mask, your body is healing.

Surgery and Implants: Last Resorts
Surgery sounds like a permanent fix-but it rarely is. Uvulopalatopharyngoplasty (UPPP), which removes excess tissue from the throat, works in only 40-60% of cases. And it’s painful. Recovery takes weeks. Many patients still need CPAP afterward.
Hypoglossal nerve stimulation (Inspire therapy) is a newer option. A small device is implanted under the skin of your chest. It senses when you breathe in and sends a tiny pulse to the nerve that controls your tongue, keeping it from blocking your airway. Studies show it reduces AHI by 79%. But it costs around $35,000 out-of-pocket, requires major surgery, and isn’t covered by most insurers. It’s reserved for severe OSA patients who’ve failed CPAP.
Who Benefits Most From CPAP?
Not everyone with OSA gets the same benefit from CPAP. A 2022 study led by Dr. Andrey Zinchuk found something surprising: it depends on your brain.
Some people have a high arousal threshold-that means they need a bigger disruption (like a full apnea) before their brain wakes them up. For them, CPAP feels like drinking coffee. They wake up refreshed, their blood pressure drops, their memory improves.
Others have a low arousal threshold. Their brain wakes up at the slightest hint of obstruction-even if breathing resumes immediately. For them, CPAP doesn’t help much. They still feel tired. Their cognition doesn’t improve. That’s why the largest CPAP trial ever (APPLES) originally showed no benefit. It didn’t account for this.
Now, experts are starting to screen for this. If you have a low arousal threshold, CPAP might not be your best first option. Oral appliances, positional therapy, or weight loss might be better starting points.
What About Lifestyle Changes?
Yes, losing weight helps. If you’re overweight, even a 10% drop in body weight can cut OSA severity in half. Sleeping on your side instead of your back reduces apnea events by up to 50%. Avoiding alcohol and sedatives before bed also helps-these drugs relax your throat muscles even more.
Positional therapy devices like NightBalance are gaining traction. They vibrate gently when you roll onto your back, nudging you to sleep on your side. In studies, they cut AHI by 51% for people whose apnea is worse when lying on their back.
There’s no magic pill yet, but drugs targeting upper airway muscle tone are in early trials. For now, lifestyle changes won’t cure OSA-but they can make any treatment work better.
Choosing the Right Path
So what should you do?
- If you have severe OSA (AHI ≥ 15) and no major issues with CPAP, start with auto-CPAP. It’s the most effective.
- If you’ve tried CPAP and quit, don’t give up. Talk to your sleep doctor. Switch masks. Try heated humidification. Get fitted for a nasal pillow. You might just need a better setup.
- If you have mild to moderate OSA and hate the mask, ask about an oral appliance. It’s FDA-cleared, covered by many insurers, and has much better adherence.
- If you sleep mostly on your back and your apnea is worse in that position, try a positional therapy device. It’s non-invasive and surprisingly effective.
- If you’ve tried everything and still struggle, talk to a specialist about hypoglossal stimulation-but only after exhausting other options.
The goal isn’t to use CPAP because it’s the “gold standard.” The goal is to sleep better, feel alert, and protect your heart. There’s more than one way to get there.
What’s Next?
The future of OSA treatment is personal. Researchers are working on:
- 3D scans of your airway to predict the exact pressure you need
- CPAP machines that adjust pressure based on your heart rate and snoring sounds
- Apps that use biofeedback to train you to sleep better without machines
For now, the best treatment is the one you’ll actually use. Don’t settle for a mask that doesn’t fit. Don’t accept exhaustion as normal. Ask questions. Try alternatives. Your health depends on it.
Is CPAP the only treatment for obstructive sleep apnea?
No, CPAP is not the only treatment. While it’s the most effective for moderate to severe cases, oral appliances, positional therapy, weight loss, and even surgical options like hypoglossal nerve stimulation are valid alternatives. The best choice depends on your OSA severity, anatomy, and personal tolerance for different devices.
Why do so many people stop using CPAP?
The main reasons are mask discomfort, claustrophobia, dry mouth or nose, and air leakage-especially through the mouth. Many users also find the machine noisy or bulky to travel with. Studies show that up to 50% of users don’t wear CPAP for more than 4 hours a night, which reduces its effectiveness. Switching mask types, using heated humidification, or trying auto-CPAP can help improve comfort and adherence.
Are oral appliances as effective as CPAP?
Oral appliances are generally less effective than CPAP at eliminating apnea events, especially in severe cases. But they’re much better tolerated. While CPAP may reduce AHI to near zero when used perfectly, oral appliances typically reduce it by about half. The real advantage is adherence-people use oral appliances on 77% of nights after a year, compared to just 4-5 hours per night for CPAP. For mild to moderate OSA, this often means better long-term outcomes.
Can lifestyle changes cure sleep apnea?
Lifestyle changes alone rarely cure OSA, but they can significantly reduce its severity. Losing 10% of body weight can cut apnea events in half. Sleeping on your side instead of your back reduces events by up to 50%. Avoiding alcohol and sedatives before bed also helps. These changes work best when combined with other treatments like CPAP or oral appliances.
How do I know if I’m a good candidate for CPAP?
You’re a good candidate if you have moderate to severe OSA (AHI ≥ 15) and can tolerate wearing a mask. If you have high blood pressure, heart disease, or daytime sleepiness, CPAP is strongly recommended. However, if you have trouble with masks, claustrophobia, or mouth breathing, you may benefit more from an oral appliance or positional therapy. A sleep specialist can help determine the best fit based on your anatomy and sleep habits.






Prajwal Manjunath Shanthappa
February 4, 2026 AT 20:31Let’s be honest-CPAP is the gold standard because it’s the only thing that actually works. Anyone who says otherwise is just romanticizing discomfort. Oral appliances? Cute. They’re like giving a diabetic a lollipop and calling it a cure. The data doesn’t lie: if your AHI is above 15, you’re playing Russian roulette with your heart. And don’t get me started on ‘positional therapy’-as if sleeping on your side is going to undo decades of obesity and poor lifestyle choices. It’s not about convenience; it’s about survival.
Wendy Lamb
February 6, 2026 AT 09:32Thanks for laying this out so clearly. I’ve seen too many people give up on CPAP because they didn’t get the right mask or humidifier. A simple switch to nasal pillows or a heated hose can make all the difference. You’re not failing-you just haven’t found your fit yet. And oral appliances? Totally valid for mild/moderate cases. It’s not one-size-fits-all. Your health, your choice.
Antwonette Robinson
February 6, 2026 AT 20:23Oh wow. So the ‘alternative’ to CPAP is… a mouthguard? And people call this medicine? Next they’ll prescribe yoga for cancer. At least CPAP is a machine that *does* something. These oral things are just fancy tongue-pullers for people who can’t handle responsibility. And don’t even get me started on ‘sleeping on your side’ like that’s a real treatment. If your throat collapses when you lie down, maybe don’t lie down? Just a thought.
Ed Mackey
February 7, 2026 AT 07:48I tried CPAP for 6 months. Mask hurt my nose, leaked like crazy, and I’d wake up with my jaw sore. Switched to an oral appliance-no more leaks, no noise, I can talk with it in. My AHI went from 38 to 18, which isn’t perfect, but I’m sleeping 7 hours now instead of 3. I’d rather have half the effect and 100% compliance than the opposite. And yeah, I spelled ‘compliance’ wrong. I’m tired.
Alex LaVey
February 8, 2026 AT 18:13This is one of the most balanced, human takes on sleep apnea I’ve ever read. Too many people treat this like a moral failure-‘if you just tried harder, you’d use CPAP.’ But sleep isn’t about willpower. It’s about finding what fits your body, your life, your sanity. I’ve seen patients cry because they felt broken for not tolerating the machine. They’re not broken. The system is. Thank you for validating that alternatives aren’t failures-they’re adaptations.
Joseph Cooksey
February 9, 2026 AT 17:31Let me just say this, with the full weight of medical literature and personal experience: the entire CPAP industry is a $10 billion racket built on the backs of people too exhausted to fight back. They sell you a $2,000 machine, then charge you $100 a month for ‘supplies’-tubes, filters, masks, humidifier pods, you name it-and then act shocked when you quit. Meanwhile, oral appliances cost $1,500 upfront, last five years, and you can take them to the beach. And don’t even get me started on how insurance companies treat sleep apnea like a lifestyle choice rather than a neurological and anatomical disorder. The fact that we’re still having this conversation in 2025 is a national embarrassment. We’ve got the tech to map airways in 3D, yet we’re still forcing people into plastic masks like medieval torture devices. Shameful.
Justin Fauth
February 10, 2026 AT 13:40CPAP is American medicine at its finest: overengineered, overpriced, and undercomfortable. We’re talking about a device that costs more than a used car and makes you feel like a cyborg. Meanwhile, in countries with real healthcare, they just tell you to lose weight, sleep on your side, and maybe get a mouthpiece. No machines. No apps. No insurance drama. We turned a simple physiological problem into a tech nightmare. And now we act like anyone who doesn’t use CPAP is lazy? Please. I’ve seen guys in India sleep through the night with a pillow between their shoulders and no machine. We’ve lost the plot.
Daz Leonheart
February 11, 2026 AT 22:41I was skeptical about the oral appliance at first, but after three months, I’m not going back. I used to wake up 5 times a night. Now I sleep through. My wife says I stopped snoring. My doctor says my AHI is down. It’s not perfect, but it’s mine. And I don’t have to unplug it every morning. That’s worth more than I can say.
Mandy Vodak-Marotta
February 13, 2026 AT 07:41Okay, real talk-I used to be the person who mocked CPAP users for dragging their machines everywhere. Then I got diagnosed. I tried CPAP for two weeks. I cried. I hated it. I felt like I was sleeping with a vacuum cleaner taped to my face. I switched to an oral appliance, got fitted by a dentist who actually listened, and now I travel with it in my toothbrush case. I still have apnea, but I’m not exhausted all the time. And honestly? I feel like I finally got to choose my own treatment instead of being told what I ‘should’ do. That’s the real win. The tech is cool, sure-but what matters is that I’m sleeping. And I’m not alone in this. So many of us are just trying to get through the night without feeling like a science experiment.