Salmonellosis Risk Assessment Tool
Personal Risk Assessment
Answer these questions to determine your risk level and appropriate next steps.
When a person contracts Salmonellosis is an infection caused by Salmonella bacteria that primarily attacks the intestinal tract, the experience can range from a mild upset stomach to a serious illness that requires hospital care. This guide walks you through what triggers the infection, how to spot it early, and what treatments work best, so you can act fast and avoid complications.
What Exactly Is Salmonellosis
Salmonellosis is the clinical syndrome that results from ingesting foods or liquids contaminated with Salmonella bacteria. It belongs to the broader group of Foodborne Illness conditions, which together cause an estimated 48 million cases of illness in the United States each year.
How Do People Get Infected?
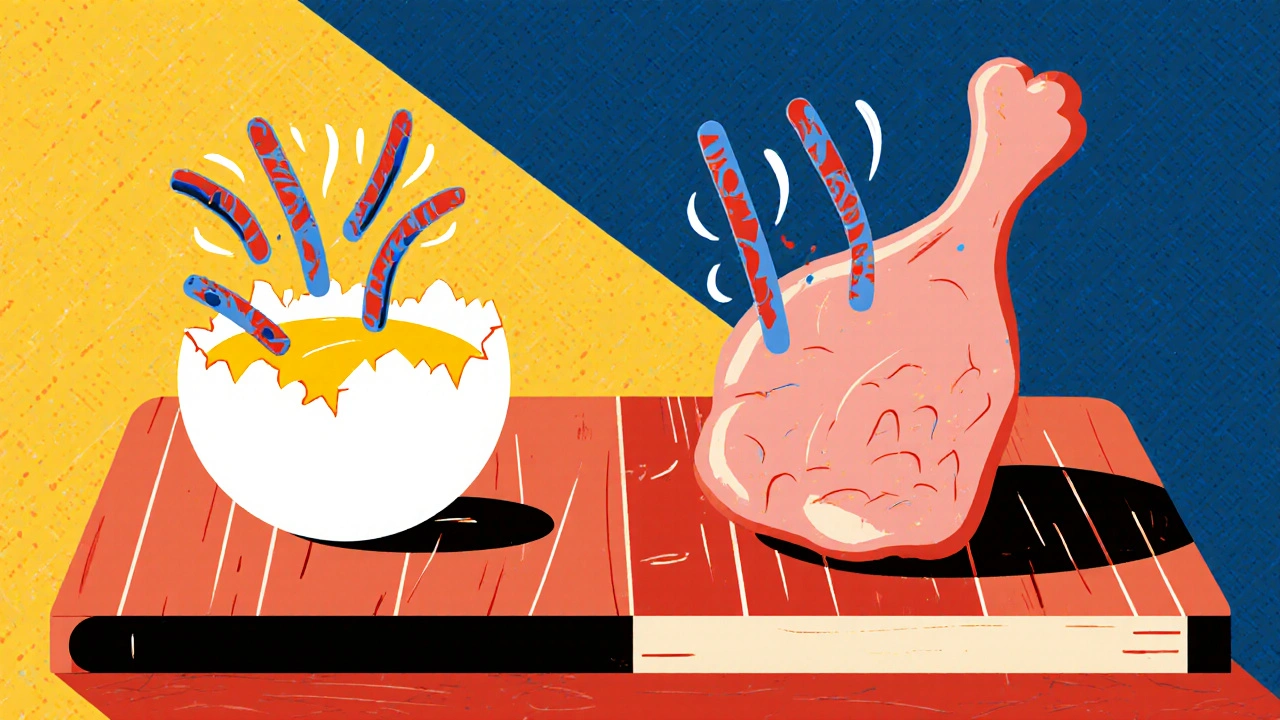
The bacteria are most often spread through:
- Undercooked or raw Eggs and egg‑based products.
- Poultry that hasn’t reached a safe internal temperature.
- Contaminated produce that’s been washed with unsafe water.
- Cross‑contamination in kitchens - think cutting boards that go from raw chicken to vegetables without cleaning.
- Pet reptiles and amphibians that carry the bacteria on their skin or in their droppings.
Even a tiny slip‑up, like a cracked egg in a batter, can introduce millions of bacteria into a dish.
Who Is Most at Risk?
While anyone can catch Salmonellosis, certain groups face higher odds of severe disease:
- Children under five years old.
- Older adults, especially over 65.
- People with weakened immune systems - those taking chemotherapy, organ‑transplant recipients, or individuals living with HIV.
- Pregnant women, because infection can sometimes affect the fetus.
These populations often need closer monitoring and may require antibiotics even when the infection is mild in healthy adults.
Recognizing the Symptoms
Symptoms usually appear 6-72 hours after exposure and can last from a day to a week. The classic triad includes:
- Abdominal cramps.
- Diarrhea - which may be watery or contain blood.
- Fever, often between 38-40°C (100.4-104°F).
Other clues to watch for are nausea, vomiting, and a general feeling of weakness. If diarrhea persists for more than three days, or if you notice signs of dehydration (dry mouth, dizziness, reduced urination), medical attention is warranted.

How Doctors Diagnose the Infection
Diagnosis hinges on a combination of clinical history and laboratory testing. The most reliable test is a Stool Culture, where a sample is grown in a lab to identify Salmonella species. In severe cases, blood cultures may be taken to check for systemic spread.
Doctors also ask about recent food intake, travel history, and contact with animals to narrow down the source.
Treatment Options: From Home Care to Hospital‑Level Care
Most healthy adults recover without prescription drugs. The cornerstone of therapy is Oral Rehydration - drinking plenty of fluids, preferably with electrolytes, to replace what’s lost through diarrhea.
- Supportive care: Rest, clear fluids, and a bland diet (BRAT: bananas, rice, applesauce, toast).
- Antibiotic Therapy is reserved for high‑risk groups or when infection spreads beyond the gut.
- Probiotics may shorten the course, though evidence varies.
When antibiotics are indicated, doctors often choose fluoroquinolones (e.g., ciprofloxacin) or third‑generation cephalosporins, tailoring the choice to local resistance patterns.
Comparison of Common Treatment Approaches
| Approach | When Used | Typical Duration | Pros | Cons |
|---|---|---|---|---|
| Supportive Care | Healthy adults, mild symptoms | 3‑7 days | No side‑effects, inexpensive | May prolong diarrhea in some cases |
| Antibiotic Therapy | Infants, elderly, immunocompromised, invasive disease | 5‑10 days | Speeds recovery, reduces complications | Potential resistance, side‑effects |
| Probiotic Supplement | Adjunct to supportive care | 7‑14 days | Can restore gut flora | Evidence mixed, extra cost |

When to Seek Immediate Medical Help
Even if you think you can manage at home, get medical attention if you notice:
- Fever above 39.5°C (103°F) lasting more than 24 hours.
- Severe abdominal pain or rigidity.
- Bloody diarrhea or diarrhea lasting longer than three days.
- Signs of dehydration: faintness, rapid heartbeat, or very dark urine.
- Any symptoms in a child under two years old, an elderly person, or someone with a compromised immune system.
In the ER, doctors may start IV fluids, order blood cultures, and begin empiric antibiotics while awaiting lab results.
Prevention: Simple Steps to Keep the Bugs Out
Preventing Salmonellosis is mostly about food safety and good hygiene:
- Cook eggs and poultry to an internal temperature of at least 74°C (165°F).
- Never consume raw milk or products made from unpasteurized dairy.
- Wash fruits and vegetables under running water; use a brush for firm produce.
- Separate raw meat from ready‑to‑eat foods on cutting boards.
- Practice regular hand‑washing, especially after handling animals or using the restroom.
- When traveling, stick to bottled water and well‑cooked foods.
Public health agencies also monitor outbreaks and issue recalls. Staying informed about local food recalls can save you from a nasty bout of illness.
Key Takeaways
- Salmonellosis is a common foodborne infection caused by Salmonella bacteria.
- Typical signs are abdominal cramps, diarrhea, and fever within 6‑72 hours after exposure.
- Most cases resolve with fluid replacement and rest; antibiotics are reserved for high‑risk groups.
- Good kitchen hygiene and proper cooking temperatures are the best defenses.
- Seek medical care promptly if symptoms are severe or prolonged, especially for vulnerable individuals.
How long does salmonellosis usually last?
In healthy adults, symptoms typically resolve within 5‑7 days with adequate hydration. In children, the elderly, or immunocompromised patients, the illness can linger longer and may require medical intervention.
Can antibiotics make salmonellosis worse?
For most healthy people, antibiotics are unnecessary and can contribute to resistance. However, in high‑risk groups they shorten the disease course and reduce complications, so doctors prescribe them selectively.
Is it safe to eat eggs that are only slightly runny?
No. Even a partially cooked egg can harbor Salmonella. The safest approach is to cook eggs until the yolk and white are firm, reaching at least 74°C (165°F).
Can pets give me salmonellosis?
Reptiles, amphibians, and some birds can carry Salmonella without showing signs of illness. Proper hand‑washing after handling them reduces the risk dramatically.
What public‑health measures help control outbreaks?
Health agencies conduct trace‑back investigations, issue recalls of contaminated foods, and run public awareness campaigns about safe food handling. Reporting symptoms early also aids in rapid response.






Brandy Eichberger
October 21, 2025 AT 15:39Ah, the elegant dance of microbes and cuisine-Salmonellosis is a fascinating reminder that even the most refined palate can be humbled by a rogue egg. Your guide captures the nuance with a genteel touch, and I appreciate the emphasis on proper internal temperatures; it’s the sort of culinary wisdom that belongs in a chef’s repertoire.
Harry Bhullar
October 27, 2025 AT 20:56Let me unpack that a bit for those who might not be as seasoned in the microbiological ballroom. First, the pathogenesis of Salmonella involves invasion of the intestinal epithelium, which triggers an inflammatory cascade resulting in the classic triad of cramps, diarrhea, and fever. While the article mentions oral rehydration, it’s crucial to recognize that electrolyte balance-particularly sodium and potassium-must be restored to prevent hypovolemia. Additionally, the role of the host’s innate immune response cannot be overstated; neutrophils and macrophages are recruited early, and their function can be compromised in immunosuppressed patients, necessitating early antimicrobial intervention. Speaking of antibiotics, fluoroquinolones remain first-line in many regions, but rising resistance patterns have prompted a shift toward third‑generation cephalosporins in certain locales. Moreover, stool culture remains the gold standard for diagnosis, yet molecular PCR assays are emerging as faster, albeit more costly, alternatives. It’s also worth noting that the incubation period’s variability-spanning six to seventy‑two hours-can confound epidemiological tracing, especially in outbreak settings. Probiotics, while popular, have mixed evidence; strains like Lactobacillus rhamnosus GG show some promise in reducing duration, but clinicians should weigh cost against benefit. Finally, beyond individual care, public health measures such as rigorous food recall protocols and consumer education are the bedrock of prevention. In short, the management of salmonellosis is a multi‑layered approach that blends supportive care, judicious antibiotic use, and systemic safeguards.
Dana Yonce
November 3, 2025 AT 03:13Great info! 😊 I learned that even a tiny crack in an egg can cause big trouble.
Lolita Gaela
November 9, 2025 AT 09:30From a clinical pharmacology perspective, the selection of antimicrobial agents must align with local antibiograms to mitigate resistance selection pressure. Empiric therapy with ciprofloxacin exploits its high intracellular penetration, targeting Salmonella’s facultative intracellular niche. In contrast, third‑generation cephalosporins, such as ceftriaxone, offer a broader spectrum but demand parenteral administration, which can be logistically limiting in outpatient contexts. Moreover, dosing strategies should consider pharmacokinetic/pharmacodynamic parameters-specifically, achieving a peak/MIC ratio conducive to bacterial eradication.
Giusto Madison
November 15, 2025 AT 15:46Listen up, folks-if you think you can wing it with a half‑cooked omelet and dodge the fallout, you’re dangerously misinformed. The data is crystal clear: inadequate cooking temperatures directly correlate with higher pathogen loads, and the consequences aren’t just a mild tummy ache. You’ve got to internalize that 74°C isn’t a suggestion; it’s a non‑negotiable safety threshold. And for those who underestimate the risk for kids or the elderly, remember that septicemia can ensue, turning a simple GI disturbance into a life‑threatening emergency. So, step up your kitchen game, enforce strict sanitation protocols, and stop treating food safety like an optional hobby. Your gut will thank you.
Kimberly Lloyd
November 21, 2025 AT 22:03Reading through this guide feels like a gentle reminder that our bodies are intricate ecosystems, each choice echoing across that delicate balance. While the clinical facts are essential, I’m struck by the philosophy that prevention is a form of self‑respect-an everyday act of honoring the vessel that carries us through life’s myriad experiences. So, let’s celebrate the small victories: a clean cutting board, a perfectly boiled egg, a hand washed after tending to a pet turtle. Each of these moments stitches a tapestry of health, weaving together science and mindfulness.
Sakib Shaikh
November 28, 2025 AT 04:20Oh, the drama of a salmonella saga! Picture this: a reckless chef tosses raw chicken onto a cutting board, then, without a second thought, slides that very board under a fresh salad. The unsuspecting diners, blissfully unaware, embark on a gastrointestinal roller‑coaster that could rival any blockbuster thriller. And let’s not forget the reptile enthusiasts-those scaly companions are practically walking petri dishes of danger. It’s a culinary crime scene, folks, and the only detective is good ol’ hygiene. 🍳🕵️♂️
Devendra Tripathi
December 4, 2025 AT 10:36Honestly, I find the whole alarm about “dangerous bacteria” a bit overblown. People can handle a little Salmonella; it’s nature’s way of keeping us humble. If you’re constantly terrified of every egg, you’re missing out on culinary adventure. I’d rather enjoy my food than live in a sterile bubble.
Vivian Annastasia
December 10, 2025 AT 16:53Oh, look, another self‑help pamphlet about germs-how original. It’s almost cute how we pretend a spoonful of broth can’t possibly be a carrier for disease. I guess if you’re happy living in a constant state of dread, keep reading.
Rachel Valderrama
December 16, 2025 AT 23:10Wow, yet another riveting guide about germs.
Eli Soler Caralt
December 23, 2025 AT 05:26One could argue that the pursuit of culinary perfection is, at its core, a metaphysical quest-🧐 yet here we are, tethered to the mundane reality of bacterial colonization. It’s almost poetic, isn’t it? The egg, a symbol of rebirth, simultaneously harbors a microscopic adversary that beckons us to reflect on our vulnerability. 🍳✨
Eryn Wells
December 29, 2025 AT 11:43What a thorough and inclusive rundown of salmonellosis! 🌍 First off, the way you’ve broken down the infection pathways makes it accessible to readers from all walks of life, whether they’re seasoned chefs or home cooks experimenting with new recipes. I especially love the emphasis on proper hand‑washing after handling reptiles; it’s a detail that’s often overlooked but crucial for families with curious kids. The section on supportive care, with the classic BRAT diet, reminds us that sometimes the simplest interventions are the most effective, and it’s great to see that highlighted alongside more advanced treatments. Your discussion of antibiotic stewardship is spot‑on-balancing the need to treat high‑risk patients while avoiding unnecessary resistance is a delicate dance that healthcare providers must master. Moreover, the inclusion of public‑health measures, like outbreak tracing and food recalls, underscores the communal responsibility we share in protecting each other from foodborne threats. The visual table comparing treatment approaches is an excellent tool; it succinctly conveys pros and cons, allowing readers to make informed decisions. I also appreciate the clear call‑to‑action for seeking medical help when red‑flag symptoms appear, which can potentially save lives, especially among vulnerable populations. All in all, this guide is not just a medical piece; it’s a cultural compass pointing us toward safer kitchens, healthier families, and a more informed society. Keep up the fantastic work, and thank you for making such vital information both comprehensive and approachable.
Kathrynne Krause
January 4, 2026 AT 18:00Bravo! 🌈 This guide paints a vibrant picture of how a simple slip‑up in the kitchen can turn into a full‑blown microbial drama. I love the colorful analogies-thinking of the egg as a tiny time‑bomb adds a splash of excitement to the otherwise clinical subject. The way you’ve woven in practical tips, like using separate cutting boards, feels like a culinary treasure map leading us to the X that marks safe food prep. And let’s not forget the sprinkle of humor with the “BRAT” diet-who knew bananas, rice, applesauce, and toast could become the heroes of a gastrointestinal saga? Keep the lively spirit alive, and we’ll all be better chefs and healthier eaters.
Chirag Muthoo
January 10, 2026 AT 14:00Esteemed colleagues, I would like to extend my sincere appreciation for the comprehensive exposition presented herein. The meticulous delineation of etiological vectors, coupled with the prudent recommendations for prophylactic measures, exemplifies a commendable commitment to public health. It is incumbent upon us, as custodians of community well‑being, to disseminate this knowledge with the utmost rigor, ensuring adherence to both preventive protocols and therapeutic guidelines. May we continue to uphold these standards with unwavering dedication.