Warfarin: What It Is, How It Works, and What You Need to Know
When you take warfarin, a prescription blood thinner that stops dangerous clots from forming in your veins and arteries. Also known as Coumadin, it’s been used for over 70 years and remains one of the most common anticoagulants worldwide. But warfarin isn’t like other pills. You can’t just take it and forget it. It demands attention—because even small changes in your diet, other meds, or health can throw off its balance and put you at risk.
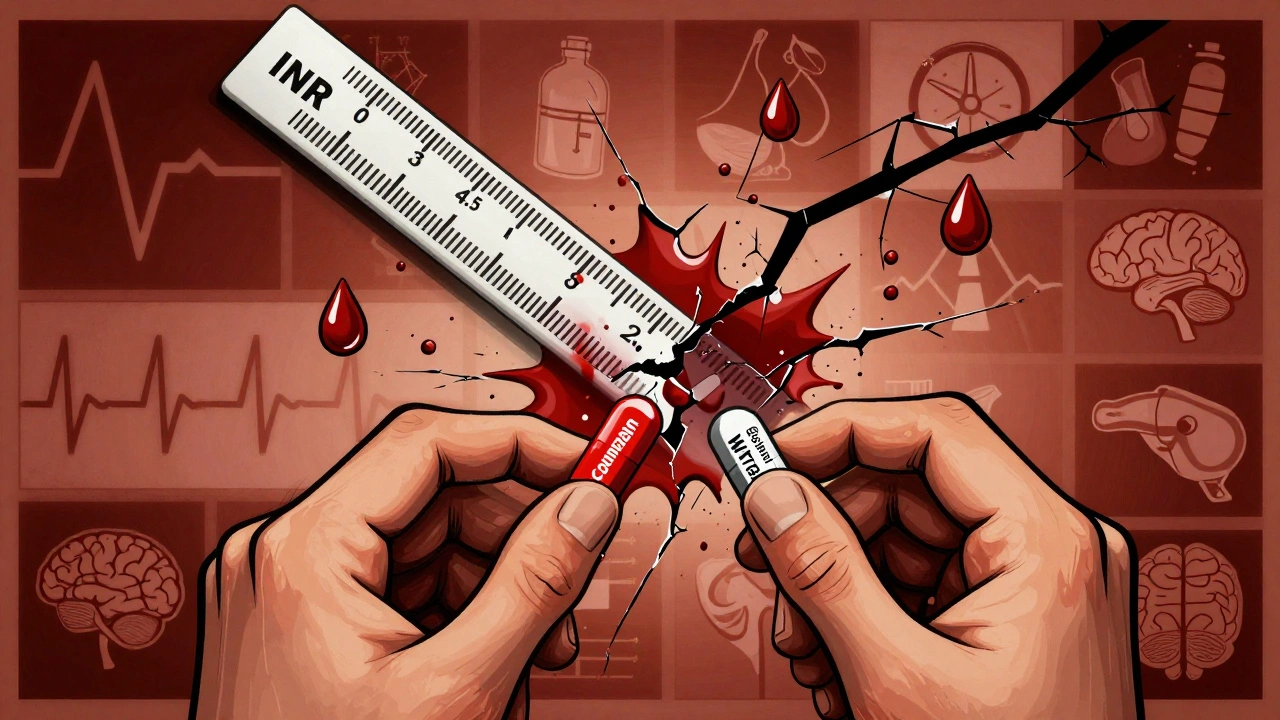
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. That’s why foods high in vitamin K—like kale, spinach, broccoli, and Brussels sprouts—can make it less effective. It’s not about avoiding them entirely, but keeping your intake steady. One day you eat a big salad, the next you skip it, and your INR (the test that measures how long your blood takes to clot) can swing dangerously. Your doctor checks your INR regularly to keep it in the safe zone, usually between 2 and 3 for most people. If it’s too low, you’re at risk for clots. Too high, and you could bleed internally without warning.
Warfarin also interacts with dozens of other drugs. Antibiotics like amoxicillin or ciprofloxacin can make it stronger. Some painkillers, like ibuprofen, increase bleeding risk. Even herbal supplements like garlic, ginkgo, or Coenzyme Q10, a supplement sometimes used for heart health and energy production. Also known as CoQ10, it can interfere with how warfarin works. That’s why it’s so important to tell every doctor, pharmacist, and even your dentist that you’re on warfarin—before they give you anything new.
People on warfarin often need to plan ahead for surgeries, dental work, or even minor procedures. Unlike newer blood thinners, warfarin can’t be reversed instantly. That’s why timing matters. You might need to stop it days before a procedure, or your doctor might use vitamin K or fresh plasma to counteract it in an emergency. There’s no one-size-fits-all approach. Your history, age, kidney function, and other meds all shape your plan.
And it’s not just about the pill. Warfarin’s effectiveness depends on how consistently you take it. Miss a dose? Take two to catch up? That’s a recipe for trouble. Many people use medication timers and apps, digital tools designed to send reminders and track when pills are taken. Also known as pill reminder apps, they to stay on schedule. These tools don’t replace your doctor’s advice, but they help you stay in control.
What you’ll find in the posts below isn’t just a list of articles—it’s a practical guide to living safely with warfarin. You’ll see how it connects to other meds you might be taking, how to avoid dangerous interactions with supplements, why lab tests like INR are non-negotiable, and how to handle travel, diet changes, or surgery without putting yourself at risk. Whether you’re just starting warfarin or have been on it for years, these posts give you the real-world details you won’t get from a pamphlet.