When a life-saving drug costs $10,000 a year and only one company holds the patent, what happens when thousands of people can’t afford it? That’s where compulsory licensing comes in - a legal tool that lets governments step in and let others make the drug, even if the patent holder says no.
What Exactly Is Compulsory Licensing?
Compulsory licensing isn’t about stealing patents. It’s about balancing rights. Under international law, patent holders get exclusive control over their inventions for a set time - usually 20 years. But that exclusivity isn’t absolute. If the public needs access - especially during a health crisis - governments can authorize someone else to produce the product without the patent owner’s permission. All they have to do is pay fair compensation.
This isn’t new. The idea was written into the 1883 Paris Convention and later locked in by the 1994 TRIPS Agreement under Article 31. That’s the global rulebook. It says compulsory licenses must be for domestic use, paid for fairly, and only used after trying to get a voluntary license first - unless there’s an emergency.
When Do Governments Use It?
Most of the time, it’s for medicines. Between 2000 and 2020, 95% of all compulsory licenses reported to the WTO were for drugs. Think HIV antivirals, cancer treatments, and now, during the pandemic, vaccines and antivirals.
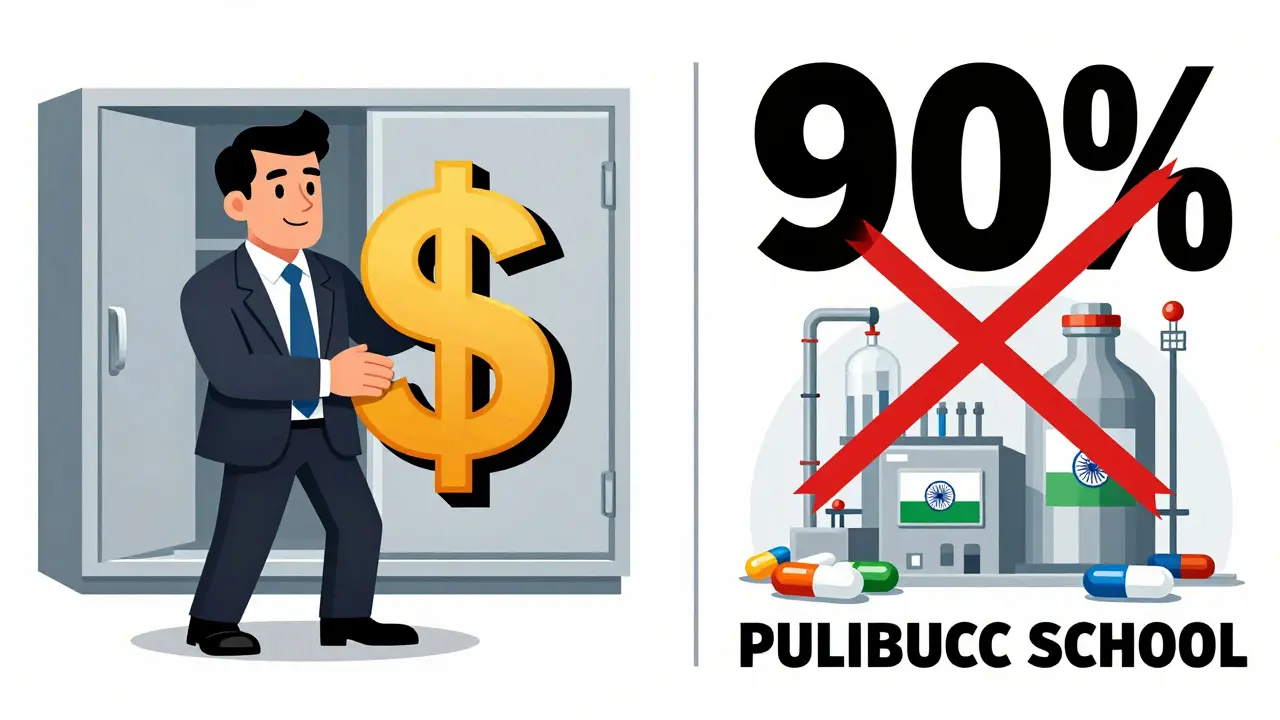
Thailand did it in 2006 for HIV drugs. They slashed the price of lopinavir/ritonavir from $1,200 a year to $230. Brazil did the same for efavirenz, dropping the cost from $1.55 per tablet to $0.48. India issued 22 compulsory licenses for cancer drugs between 2005 and 2021. In each case, generic manufacturers stepped in and made the medicine cheaper - sometimes by 90%.
During the early days of COVID-19, over 40 countries - including Canada, Germany, and Israel - prepared to issue compulsory licenses for testing kits, treatments, and vaccines. Even though many didn’t end up using them, the threat alone pushed drugmakers to lower prices or offer voluntary deals.
How It Works in Different Countries
The rules vary wildly. In the U.S., there are three main paths:
- Section 1498: The federal government can use any patented invention - say, a vaccine tech - and pay damages later. This has been used since the 1940s, mostly for military gear. Only 10 cases total between 1945 and 2020.
- March-in rights: If a drug was developed with federal research money (like from NIH), the government can force a license if the company isn’t making it available. The NIH has received 12 requests since 1980. They’ve denied every single one, saying the company was "doing enough."
- Environmental laws: The Clean Air Act lets the government license patents needed to meet pollution standards. Rare, but it’s there.
In Europe, it’s up to each country. Germany’s law allows it for public interest - but they’ve never used it. France and Spain have used it for health emergencies. Spain passed a law in 2020 that let them skip the "try to negotiate first" step during the pandemic.
India’s system is the most active. Their Patents Act requires applicants to prove they tried to get a voluntary license, show a public health need, and have the ability to make the drug. The process takes 18-24 months. Still, they’ve issued 22 licenses - more than any other country.
What’s the Catch?
It’s not a free pass. Compulsory licensing comes with real trade-offs.
First, the patent holder gets paid. How much? That’s where things get messy. In the U.S., courts use something called the "Georgia-Pacific factors" - 15 criteria like royalty rates for similar licenses. In India, they use a fixed formula: 6% of net sales. That’s what happened with Nexavar, the kidney cancer drug. Natco Pharma paid Bayer 6% of what they made, not the full market price.
Second, there’s the fear of chilling innovation. A 2018 study in the Journal of Health Economics found that countries with active compulsory licensing programs saw a 15-20% drop in pharmaceutical R&D investment. Big drug companies argue that if they can’t protect their profits, they won’t invest in new drugs.
But here’s the counter: the threat of compulsory licensing has already forced voluntary price cuts. Dr. Brook Baker, a law professor, says that since 2000, 90% of HIV drugs in developing countries became cheaper because companies feared governments would step in. The license itself wasn’t needed - just the possibility.
Then there’s the legal mess. Bayer spent eight years fighting India’s Nexavar license. The case went all the way to the Delhi High Court. That kind of delay costs time, money, and lives.
Who Benefits?
Not drug companies. Not usually. The real winners are patients and generic manufacturers.
Teva Pharmaceutical made $3.2 billion extra between 2015 and 2020 from drugs produced under compulsory licenses. Generic makers in India, Brazil, and South Africa now have the legal right to produce affordable versions of drugs that were once out of reach.
And it’s not just medicines. The 2017 Marrakesh Treaty lets countries issue compulsory licenses so blind or visually impaired people can access books in accessible formats. Canada and India have used it.
But here’s the kicker: 60% of low- and middle-income countries don’t have the legal or technical capacity to even start the process. They have the law on paper, but no lawyers, no patent experts, no way to navigate the bureaucracy.

What’s Changing Now?
The biggest shift came in June 2022, when the WTO agreed to a temporary waiver on COVID-19 vaccine patents. For the first time, developing countries could produce vaccines without asking permission - as long as they’re used for domestic needs. But so far, only 12 facilities in 8 countries have been approved to use it. The system is still too slow, too complex.
The EU is pushing new rules. Their 2023 Pharmaceutical Strategy says if a company doesn’t offer fair licensing terms within 30 days, the government can skip negotiations and issue a license immediately. That’s a big change.
The WHO is also drafting a Pandemic Treaty. One draft article says: when a global health emergency is declared, essential health products - vaccines, drugs, diagnostics - should be automatically licensed. No waiting. No negotiation. Just access.
Industry analysts predict a 40% increase in compulsory licensing between 2023 and 2028. Why? Antimicrobial resistance. Climate-related health threats. The next pandemic is coming. And governments are realizing: patents can’t be allowed to stand in the way of survival.
Is It Fair?
Some say it’s theft. Others say it’s justice.
Drugmakers argue that innovation needs protection. Without patents, no one would spend $2.6 billion and 10 years developing a new drug. That’s true. But it’s also true that 10% of the world’s population gets 80% of the world’s medicines. Millions die because the price tag is too high.
Compulsory licensing doesn’t kill innovation. It forces it to serve people, not just profits. The most successful cases - like Thailand, Brazil, India - didn’t destroy companies. They forced them to negotiate. To lower prices. To make deals.
The real question isn’t whether it’s legal. It’s whether we can afford not to use it.
What’s Next?
For now, compulsory licensing remains a tool of last resort. But it’s becoming less of a threat and more of a standard part of the public health toolkit. Countries that build strong, transparent systems - clear rules, fast decisions, fair pay - will be the ones ready for the next crisis.
If you’re in a country where a life-saving drug is unaffordable, the law may already give you a path. It’s not easy. It’s not quick. But it’s there.







Chelsea Harton
January 18, 2026 AT 10:23so like… if a drug costs 10k but generics make it 230, why are we still having this convo? people die because of greed. end of story.
Travis Craw
January 19, 2026 AT 00:26i get that patents are supposed to incentivize innovation, but when people cant even buy insulin, something’s broken. maybe the system needs a reboot, not just tweaks.
Christina Bilotti
January 20, 2026 AT 23:52oh wow, a *legal tool*? how revolutionary. next you’ll tell me the sky is blue and water is wet. the fact that we even debate this is proof we’ve lost our moral compass. 🤦♀️
brooke wright
January 22, 2026 AT 22:17have you ever tried navigating the legal system in a country with no patent lawyers? it’s like trying to assemble ikea furniture blindfolded while being yelled at. the law exists, sure-but the access? nonexistent. and that’s the real tragedy.
vivek kumar
January 24, 2026 AT 18:37India issued 22 compulsory licenses for cancer drugs. Not because we’re anti-patent, but because people are dying. We followed the TRIPS rules, paid fair royalties, and saved lives. The WHO should study our model-not the pharmaceutical lobbyists.
Stephen Tulloch
January 25, 2026 AT 08:06can we just admit that Big Pharma is basically a cartel with a PR team? 🤡 they patent everything from peanut butter to toenail clippings. if they really cared about innovation, they’d invest in prevention, not pricing strategies. also, emoji for the win: 💊💸
Melodie Lesesne
January 27, 2026 AT 07:48the fact that we even need to talk about this is sad. if a drug saves lives, it should be treated like clean water or fire extinguishers-not a luxury item. i’m just glad some countries are stepping up.
Corey Chrisinger
January 28, 2026 AT 14:10patents were never meant to be weapons against mortality. they were designed to reward innovation, not to create monopolies over human survival. if a company can’t adapt to a world where health is a right, not a privilege, maybe they shouldn’t be in this business.
Bianca Leonhardt
January 28, 2026 AT 17:08you think this is justice? it’s theft dressed up as policy. without profit, there’s no research. no research, no cures. you want cheap drugs? fine. but don’t be surprised when the next breakthrough never happens.
Riya Katyal
January 28, 2026 AT 19:44ohhh so india’s the hero now? cute. they copy everything. even their ‘generic’ drugs are just reverse-engineered with a different label. innovation? nah. they just wait for someone else to do the hard work.
swarnima singh
January 29, 2026 AT 15:12it’s not about money. it’s about soul. when you charge $10k for a drug that costs $50 to make… you’re not a company. you’re a vampire. sucking blood from the sick. i don’t care if you ‘invented’ it. if it doesn’t save lives, it’s just a pretty lie.
Isabella Reid
January 30, 2026 AT 21:45the WTO waiver on vaccines was a step. but 12 facilities approved in two years? that’s not progress. that’s a glitch. we need global infrastructure, not patchwork loopholes. this isn’t a crisis of law-it’s a crisis of will.
Jody Fahrenkrug
February 1, 2026 AT 10:33my cousin needed a cancer drug last year. insurance denied it. we sold our car. still couldn’t afford it. i’m not mad at the system. i’m just… tired.
Kasey Summerer
February 2, 2026 AT 10:36so you’re telling me the guy who spent $2.6B and 10 years on a drug gets nothing? lol. yeah right. next you’ll say Elon should give away rockets because someone might need to go to Mars. 😏