When you’re told you have Crohn’s disease, it’s not just a diagnosis-it’s a life shift. This isn’t a simple stomach bug that clears up in a few days. It’s a chronic condition where your immune system turns on your own gut, causing ongoing inflammation that can lead to pain, diarrhea, weight loss, and even surgery. For decades, treatment meant steroids, immunosuppressants, and hoping for remission. But today, biologic therapy has changed everything. These targeted drugs don’t just mask symptoms-they stop the inflammation at its source.
What Makes Crohn’s Disease Different
Crohn’s disease isn’t just "bad IBS." It’s an autoimmune disorder that can attack any part of your digestive tract, from your mouth to your anus. Most often, it hits the end of the small intestine (terminal ileum) and the beginning of the colon. Unlike ulcerative colitis, which only affects the inner lining of the colon, Crohn’s digs deep-through all layers of the intestinal wall. That’s why complications like strictures (narrowing), fistulas (abnormal tunnels), and abscesses are so common. About 30-50% of people develop strictures within 10 years. One in three will get a fistula. The cause? It’s not one thing. Genetics play a big role. If you have a close relative with Crohn’s, your risk goes up. Mutations in the NOD2 gene are found in 30-40% of families with the disease. But genes alone don’t cause it. Your gut bacteria, diet, smoking, and even where you live (more common in urban, industrialized areas) all interact with your immune system. The result? Your body mistakes harmless bacteria for invaders and launches a constant, damaging attack.How Biologics Work: Targeting the Root Cause
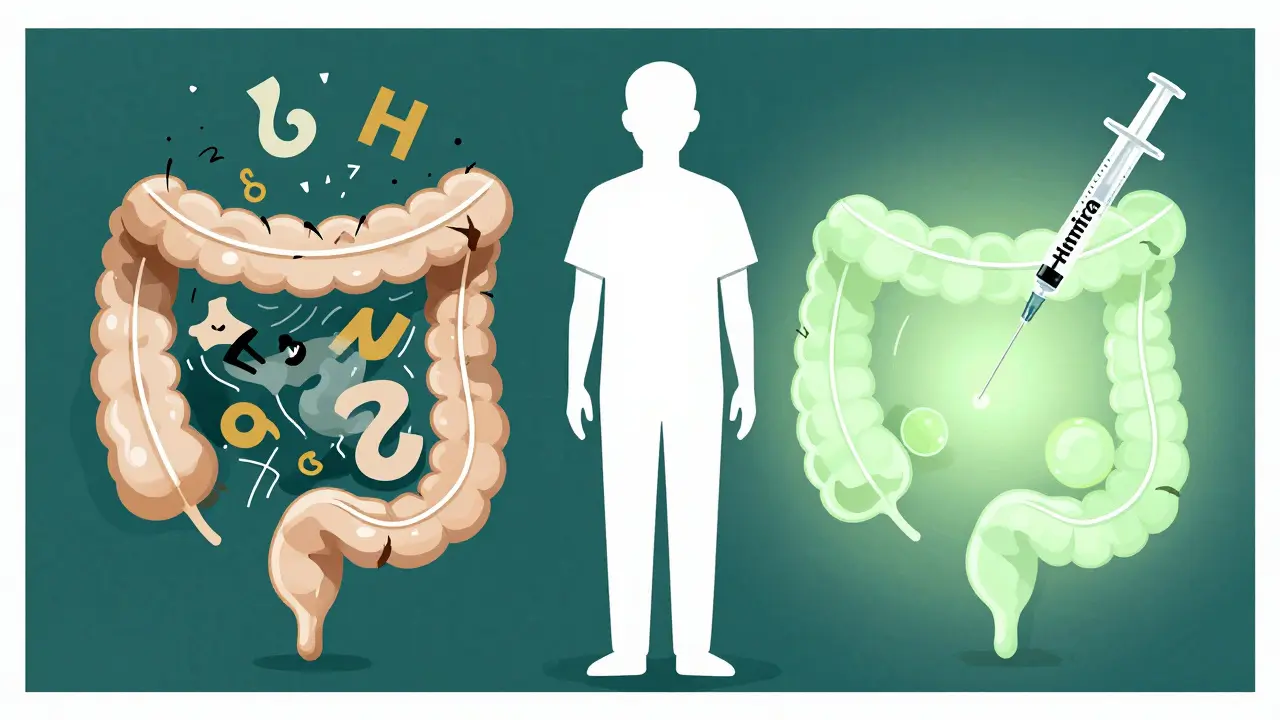
Traditional drugs like azathioprine or corticosteroids suppress your whole immune system. That’s why you’re more likely to get infections or develop liver issues. Biologics are different. They’re made from living cells and designed to hit specific parts of the inflammation chain. The most common type targets TNF-alpha-a key inflammatory protein. Drugs like infliximab (Remicade), adalimumab (Humira), and certolizumab (Cimzia) block this molecule. Think of it like cutting a wire in a bomb. No TNF-alpha, no signal to keep the inflammation going. Within weeks, many patients see fewer bowel movements, less pain, and healing of the gut lining. Studies show 30-40% of people on anti-TNF drugs go into remission, compared to just 15-20% on placebo. Then there are newer options. Vedolizumab (Entyvio) doesn’t touch the whole immune system. It blocks a specific molecule (α4β7 integrin) that only lets immune cells enter the gut. That means it’s safer for people who’ve had infections or are worried about side effects elsewhere. Ustekinumab (Stelara) targets IL-12 and IL-23, two other messengers that drive inflammation. In clinical trials, about 40% of patients on ustekinumab were in remission after just 8 weeks.Choosing the Right Biologic: It’s Not One-Size-Fits-All
Not all biologics are the same. Here’s how they stack up:| Drug Name | Type | How It’s Given | Time to Work | Remission Rate (8-12 weeks) | Annual Cost (USD) |
|---|---|---|---|---|---|
| Infliximab (Remicade) | Anti-TNF | IV infusion | 2-4 weeks | 30-40% | $40,000-$60,000 |
| Adalimumab (Humira) | Anti-TNF | Subcutaneous injection | 2-4 weeks | 30-40% | $35,000-$55,000 |
| Vedolizumab (Entyvio) | Integrin inhibitor | IV infusion | 10-14 weeks | 25-30% | $45,000-$65,000 |
| Ustekinumab (Stelara) | IL-12/23 inhibitor | Subcutaneous injection | 8 weeks | 34-44% | $50,000-$70,000 |
Anti-TNF drugs work fast but lose effectiveness over time. Up to half of patients stop responding within a year because their body builds antibodies against them. Vedolizumab doesn’t have that problem-only 4% develop antibodies versus 15-20% with anti-TNFs. But it takes longer to kick in. If you’re in a flare and need quick relief, anti-TNFs are better. If you’ve had infections or are at risk for multiple sclerosis, vedolizumab is safer.
Therapeutic Drug Monitoring: Dosing Isn’t Guesswork
One of the biggest shifts in Crohn’s care is moving from fixed doses to personalized dosing. Doctors now check drug levels in your blood. For infliximab, the sweet spot is 3-7 μg/mL. For adalimumab, it’s 5-12 μg/mL. If your levels are too low, you’re more likely to relapse. If they’re too high, you risk side effects. Studies show patients who get their doses adjusted based on blood tests are 3.5 times more likely to stay in remission. This isn’t experimental-it’s now standard at top IBD centers. If your doctor isn’t checking your levels, ask why. You’re not just taking a pill-you’re managing a precise biological tool.Real Stories: The Good, the Bad, and the Costly
On Reddit, a user named CrohnWarrior87 wrote: "After 15 bowel movements a day, infliximab brought me down to 2 in three infusions. I went from bed to work in six months." That’s the dream. But another user, IBSurvivor22, shared: "I developed lupus-like symptoms on Humira. It took six months of steroids to recover." Serious side effects like this are rare-about 1 in 100-but they happen. That’s why screening is non-negotiable. Before starting any biologic, you need tests for tuberculosis, hepatitis B, and heart health. Some drugs can reactivate old infections. Then there’s the cost. Even with insurance, copays can hit $150 per dose. A 2023 survey found 40% of patients delayed or skipped doses because they couldn’t afford it. That’s not just financial stress-it’s medical risk. Many drug companies offer patient assistance programs that cover 30-50% of out-of-pocket costs. Ask your clinic. Don’t assume you’re out of luck.What Happens When Biologics Don’t Work
If a biologic stops working, you don’t just go back to steroids. You switch. Many patients try a second biologic with a different target. For example, if adalimumab fails, switching to ustekinumab or vedolizumab often works. Studies show 40-50% of patients respond to a second-line biologic. New drugs are coming fast. Ozanimod, a pill that traps immune cells in lymph nodes, showed 37% remission in trials. Mirikizumab, which blocks just IL-23, had 40% of patients showing visible healing in the colon. These aren’t just hope-they’re near-future options.
Living With Biologic Therapy: Practical Tips
Starting biologics isn’t a one-time event. It’s a lifestyle adjustment.- If you’re on injections (Humira, Stelara), learn proper technique. Most people get comfortable after 2-3 sessions with a nurse.
- Keep a symptom tracker. Apps like MyIBDCoach help you log bowel habits, pain, and side effects-useful for doctor visits.
- Plan infusions around work. Many centers offer early morning or weekend slots.
- Don’t skip vaccines. Get the flu shot, pneumonia shot, and hepatitis B vaccine before starting. Avoid live vaccines like MMR or shingles while on biologics.
- Watch for signs of infection: fever, chills, cough, or unexplained fatigue. Call your doctor immediately.
The Future: Earlier, Smarter, Cheaper
The biggest change in the last decade? Starting biologics sooner. Ten years ago, doctors waited until medications failed. Now, if you have deep ulcers, fistulas, or a family history of surgery, experts recommend starting a biologic right away. One study showed this "top-down" approach cuts surgery risk by 50% over five years. Biosimilars-cheaper copies of biologics like infliximab-dyyb-are now widely available. They work just as well and cost 15-30% less. Insurance is slowly catching up, but you may need to push for them. The goal isn’t just to feel better. It’s to heal your gut, avoid surgery, stay off steroids, and live a full life. Biologics make that possible-for most people, most of the time.Can biologics cure Crohn’s disease?
No, biologics don’t cure Crohn’s disease. They don’t remove the underlying genetic or immune triggers. But they can induce deep remission-meaning no symptoms, no inflammation visible on scans, and no need for steroids. Many people live normal, active lives for years while on treatment. The goal is long-term control, not a one-time fix.
How long do I need to stay on biologics?
Most people stay on biologics long-term. Stopping increases the risk of flare-ups, and restarting often doesn’t work as well. Some patients who achieve deep, lasting remission may try to taper under close supervision, but this is rare and risky. Only about 10-15% can safely stop without relapsing. For most, it’s a chronic treatment, like insulin for diabetes.
Do biologics increase cancer risk?
There’s a small increased risk of certain skin cancers and lymphoma, but the overall risk remains low-about 1 in 1,000 per year. This risk is higher in older patients or those on multiple immunosuppressants. Regular skin checks and avoiding excessive sun exposure help. The bigger risk? Not treating Crohn’s. Untreated inflammation increases colon cancer risk over time. For most, the benefit of controlling inflammation outweighs the small cancer risk.
Can I get pregnant while on biologics?
Yes, many biologics are safe during pregnancy. Infliximab and adalimumab cross the placenta in the third trimester, so doctors often stop them around 30 weeks to avoid affecting the baby’s immune system. Vedolizumab and ustekinumab don’t cross as much and are often continued. Never stop without talking to your IBD team. Active Crohn’s during pregnancy carries higher risks of preterm birth and low birth weight than the medications do.
What if I can’t afford my biologic?
You’re not alone. Many drug manufacturers offer copay assistance programs that reduce monthly costs to under $50. Some nonprofits, like the Crohn’s & Colitis Foundation, provide grants for medication access. Biosimilars are now available for several drugs and cost 30-50% less. Talk to your clinic’s financial counselor-they handle this daily. Never skip doses because of cost-there are solutions.







Rob Deneke
January 17, 2026 AT 00:40Been on Humira for 3 years now. Some days are rough but I can actually plan a weekend without knowing where the nearest bathroom is. Worth every penny and every needle.
Still hate the infusion center though.
evelyn wellding
January 18, 2026 AT 18:54OMG YES THIS!! 🙌 I was in the hospital for 10 days last year and now I’m hiking with my dog. Biologics didn’t just save my health-they saved my life. Don’t give up!
Chelsea Harton
January 19, 2026 AT 22:09Life is pain. Biologics are just a bandaid on a bullet wound. But hey, at least the bullet stopped firing for now.
Nick Cole
January 20, 2026 AT 09:26People who say 'just eat better' or 'it's all stress' need to stop. This isn't a lifestyle choice. This is your immune system betraying you. Biologics are the only thing that actually treat the disease, not just the symptoms. If your doctor isn't pushing this, find a new one.
Isabella Reid
January 22, 2026 AT 05:47I love how the article mentions biosimilars. My cousin switched from Humira to a biosimilar and saved $20k a year. Same results, way less stress on the wallet. We need more transparency around pricing and access. Not everyone has good insurance.
Jody Fahrenkrug
January 22, 2026 AT 06:11Just started vedolizumab last month. Took 12 weeks to feel anything but now I’m sleeping through the night. Patience is wild.
Ryan Hutchison
January 23, 2026 AT 20:45Why do Americans pay $60k for a drug that costs $5k to make? This is why we need single-payer. In Canada, I got mine for $10 a month. You’re being ripped off.
Samyak Shertok
January 24, 2026 AT 08:39Ah yes, the great Western medical miracle. Injecting proteins into your veins to fix a problem caused by processed food, antibiotics, and existential dread. How quaint. In Ayurveda, we’d just cleanse your doshas and stop blaming your gut for your trauma.
Corey Chrisinger
January 26, 2026 AT 06:41I think about biologics like tuning a violin. Too much pressure? It breaks. Too little? It sounds off. Blood levels? That’s the tuner. We’re not just patients-we’re musicians now. And the orchestra is our immune system.
Bianca Leonhardt
January 28, 2026 AT 00:43If you’re still on steroids, you’re doing it wrong. This isn’t 2010. If your doctor hasn’t mentioned biologics by now, they’re either lazy or haven’t updated their textbooks since the Bush administration.
Travis Craw
January 28, 2026 AT 08:21I didn’t know you could check drug levels. My doc never mentioned it. Guess I’ll be asking next time. Thanks for the heads up.
Christina Bilotti
January 30, 2026 AT 06:42Of course the article mentions patient assistance programs. Because nothing says 'progress' like a billionaire pharma exec offering you a coupon to survive. The real scandal? These drugs were developed with public funding. Now we pay for the privilege.