Generic Substitution: What It Is, How It Works, and Why It Matters
When you pick up a prescription and get a different pill than what your doctor wrote, that’s generic substitution, the practice of swapping a brand-name drug for a chemically identical generic version at the pharmacy. Also known as therapeutic equivalence, it’s one of the biggest cost-savers in U.S. healthcare—saving over $445 billion in 2023 alone. This isn’t a loophole or a trick. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They work the same. They’re just cheaper.
But here’s the catch: not all substitutions are created equal. FDA approvals, the rigorous process that certifies generic drugs are bioequivalent to their brand-name counterparts are strict—but they’re not foolproof. Some generics slip through with inconsistent fillers or manufacturing flaws. That’s why you see posts about counterfeit medications, fake pills that look real but contain nothing—or worse, dangerous substances showing up in online pharmacies and even some legitimate supply chains. Pharmacists are trained to spot red flags, but you need to know how to verify your pharmacy and check if your pill is the real thing.
Generic substitution isn’t just about price. It’s about access. Medicaid programs in different states have wildly different rules on when pharmacists can switch your drug without asking your doctor. Some states require prior authorization for certain generics. Others allow automatic substitution unless you or your doctor opt out. And then there’s the issue of authorized generics—brand-name drugs sold under a generic label, identical in every way, but confusingly priced lower than the original. These aren’t fakes. They’re a business move by drug companies trying to keep market share after patents expire.
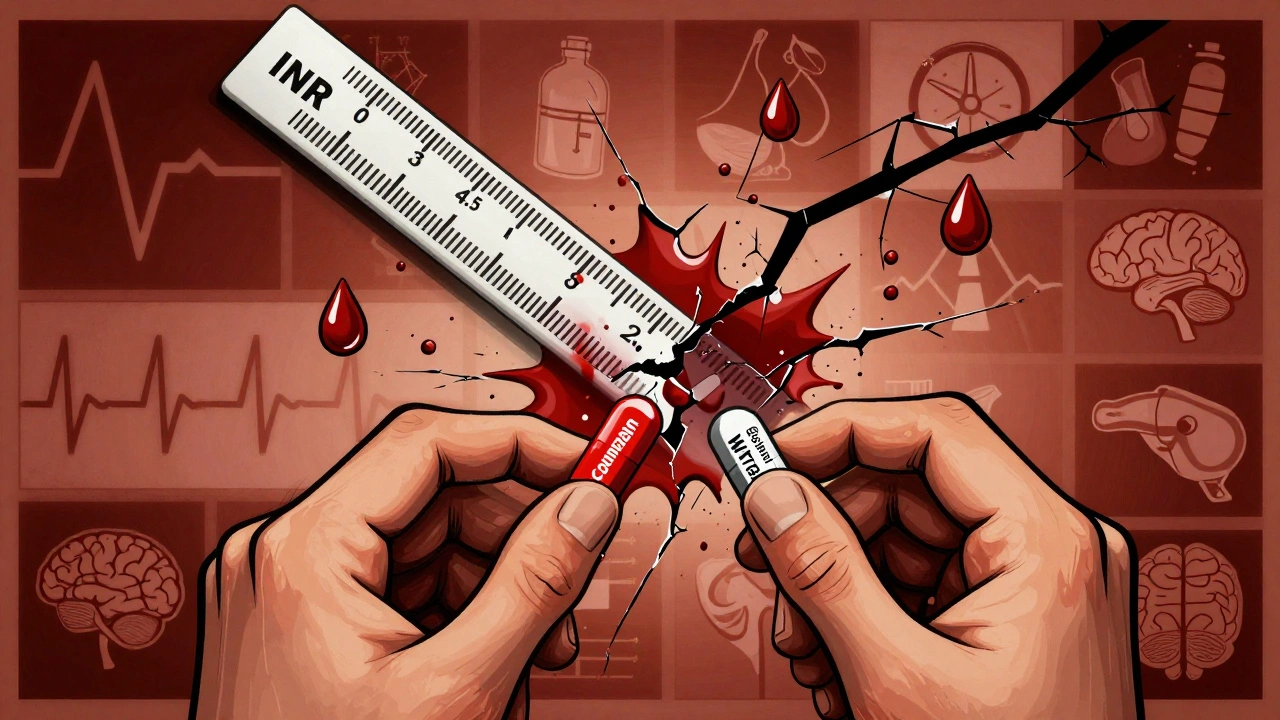
What you won’t find in most doctor’s offices is the full picture. Why does your blood pressure med work fine one month, then feel off the next? Could it be a different generic manufacturer? Why did your pharmacist call your doctor about switching your antibiotic? Because even tiny differences in inactive ingredients can affect absorption—especially with thyroid meds, seizure drugs, or blood thinners. That’s why pharmacists use FDA data, cost comparisons, and real-world evidence to talk to prescribers about when substitution is safe—and when it’s not.
And let’s not forget the people who rely on this system. Millions of Americans can’t afford brand-name drugs. Without generic substitution, many would skip doses, split pills, or go without. But if you’re handed a pill that looks different and you don’t know why, you might stop taking it altogether. That’s why understanding what’s in your bottle matters more than you think.
Below, you’ll find real-world guides on how generic drugs are made, how to spot fakes, how pharmacies verify them with barcode scans, how much money they save every year, and what to do if your state’s Medicaid program denies your generic. You’ll learn how to talk to your pharmacist, how to check if your drug is truly equivalent, and why expiration dates on generics matter just as much as on brands. This isn’t theory. It’s what’s happening in pharmacies, hospitals, and your medicine cabinet right now.