NTI Drugs: What They Are, Why They Matter, and How to Use Them Safely
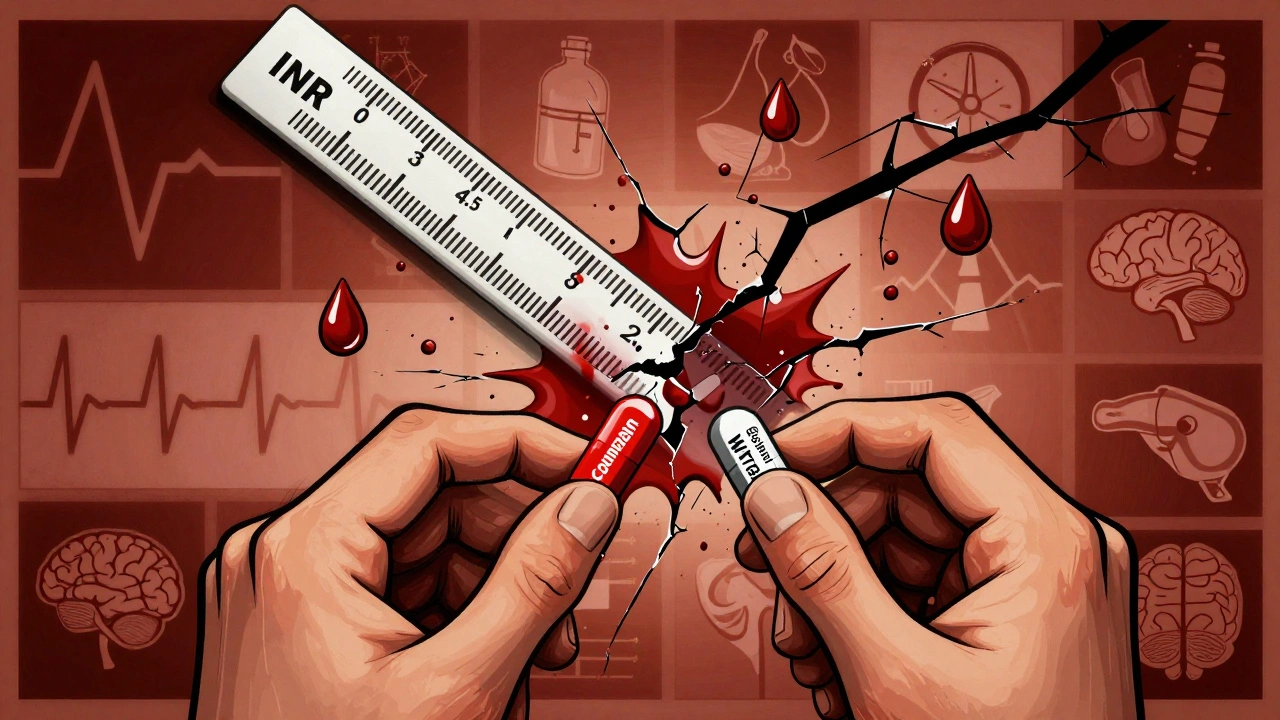
When a medication has a Narrow Therapeutic Index, a small difference in dose can lead to treatment failure or serious toxicity. Also known as NTI drugs, these medications sit on a razor’s edge—enough to heal, but just enough to harm if the dose is off by a fraction. Think of them like driving a race car: one wrong turn and you crash. Drugs like warfarin, levothyroxine, phenytoin, cyclosporine, and digoxin fall into this category. They’re not rare—millions take them daily—but most people don’t realize how tightly their safety is controlled.
NTI drugs require more than just a prescription. They demand precision. That’s why therapeutic drug monitoring, the process of measuring drug levels in the blood to ensure they stay in the safe zone is often required. A blood test isn’t optional here—it’s the only way to know if your dose is right. And it’s not just about the dose. Things like diet, other medications, liver function, and even changes in your body weight can shift how your system handles these drugs. For example, switching from one generic version of levothyroxine to another—even if both are FDA-approved—can cause your thyroid levels to swing dangerously if you’re not monitored. That’s why pharmacists and doctors track these changes closely, and why some states have strict rules about substituting NTI drugs without approval.
These drugs also play a big role in conditions where timing and consistency matter most. If you’re on immunosuppressants, medications that prevent organ rejection but leave you vulnerable to infection, even a slight drop in blood levels can trigger rejection. Too much, and you risk kidney damage or cancer. That’s why labs check tacrolimus or cyclosporine levels every few weeks. The same goes for seizure meds like phenytoin—too low, and you have a seizure; too high, and you risk brain fog, tremors, or worse. It’s not just about taking your pill. It’s about knowing your body’s response, watching for side effects, and communicating with your care team every step of the way.
And here’s the thing: NTI drugs don’t care if you’re tired, stressed, or ran out of pills last week. They react to what’s in your system—not your intentions. That’s why tools like medication timers and apps aren’t just helpful—they’re critical. Missing a dose or taking two by accident can have real consequences. Even small changes like switching from brand to generic, starting a new supplement like Coenzyme Q10, or drinking grapefruit juice can interfere with how these drugs work. That’s why your pharmacist asks so many questions. They’re not being nosy—they’re trying to keep you alive.
Below, you’ll find real-world guides on how to manage these high-risk medications safely. From how to handle interactions with supplements and antibiotics, to why barcode scanning in pharmacies matters for NTI drugs, to how Medicaid and generic substitution rules affect your access—you’ll find practical, no-fluff advice from people who’ve been there. This isn’t theory. It’s what keeps people alive every day.